News 4/5/11
Todd Rothenhaus, MD joins athenahealth as chief medical officer. He most recently served as SVP and CIO of Steward Health Care (formerly Caritas Christi Health Care).
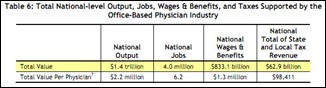
Physician offices added 7,600 jobs in March, representing a 0.3% gain. Total physician office employment is 2.3 million.
Webahn announces that its Capzule EMR is available to solo practices free of monthly charges. Capzule EMR does not display advertisements and does not require revenue sharing, so what’s the catch? The Capzule Web site says the EMR is not (yet) ONC-ATCB certified and does not offer e-prescribing. Also, the EMR does not come pre-loaded with ICD-9 or CPT codes. The “free” option is limited to solo practices, includes only one additional non-physician license, and it includes limited templates and customization options. The standard package costs $150 per month per physician and $10 per month for non-physician users.
The newest generation of doctors want salaried jobs, fewer working hours, and specialties that are conducive to family life, according to a New York Times article. At the same time, doctors are not revered by their patients like days of old. In fact, patients today are more likely to see doctors as interchangeable.
The 80-physician Doctors Clinic (WA) goes live on Sage’s online patient portal.
The Child Guidance Center of Southern Connecticut implements CareLogic Enterprise EHR by Qualifacts’. The purchase was partly funded by a $100,000 private foundation challenge grant.
About 56% of practices have not scheduled testing of the 5010 transaction set, according to MGMA. Less than 4% said they had begun testing the transaction set with health plans. Most disturbing: 23% of survey respondents didn’t know what needed to be done to their software to implement 5010.
I noticed that AAFP opened its annual EHR satisfaction survey survey. AAFP members using commercial EHRs can participate here. It’s not the most scientific survey out there (results are based on physician self-reporting rather than a random sample). Still, the results are interesting and give certain vendors the chance to brag a bit.
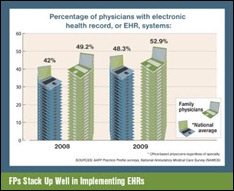
AAFP also posts a special report EHRs, which includes a number of articles on EHR use in family practices, details on the EHR incentive plan, and more. I’m not sure there is much new, but the section includes a nice variety of information all in one place.
HIT consultants say practices often underestimate the amount of training required for EHR or reduce training to save money or time. When calculating the amount of time required for training, practices and vendors should keep in mind the amount of data being abstracted from previous systems; integration needs; introduction of new hardware, especially end-user devices; and existing computer skills.
And from a different group of consultants: if you have physicians resistant to structured data capture, find a hybrid approach that blends the ability to capture required structure data elements and provides the physicians the flexibility to document in their own personal manner. The result will be increased physician adoption and better data for reporting and exchanging with other providers. Evan Steele swears he didn’t write the article, but he could have.
There’s still a lot to process about the recently proposed ACO regulations, but one thing is clear: ACOs will need solid HIT infrastructure. The regulations call for ACOs to report on 65 quality measures, so systems will need to be in place to churn out those numbers. In addition, at least 50% of an ACO’s primary care providers be EHR Meaningful Users. Another takeaway: consultants are going to win big, as providers turn to them to determine their needs and assess the value of their potential ACO participation.













Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…