It’s my honor and privilege to appear this week on HIStalk Practice while Inga and Mr. H are out enjoying spring break. I’m happy to help keep the home fires burning. Frankly, after some of the things I saw while providing emergency department coverage for Mardi Gras, I’m content to sit happily at home with my laptop and a cup of cocoa.
I did venture out this weekend to have dinner with a good friend, someone with whom I shared the wonder and agony that is Residency Training. For you non-clinicians, residency is the multi-year period after one has graduated from medical school and has a degree, but continues to train under supervision. It’s a high-stress time when you learn how to run a hospital-based practice as efficiently as possible. Unfortunately, except for a handful of programs, they don’t teach you much of anything about how to run an office-based practice.
My friend finished residency and joined a small private specialty practice. The scattered topics we hit during dinner and drinks reminded me how widely varied physicians’ experiences are with regards to healthcare IT and the various state and federal rules and regulations, let alone Meaningful Use. There were some random things I mentioned about liking or not liking in the EHR, such as logging samples, and we discovered that her practice is blissfully unaware of some of the things that are looming.
She’ll be deploying an EHR in the coming months, trying to get her piece of the federal pie, and I’m sure I’ll be hit for many curbside consults in the future. As long as she pays the bar bill, that’s OK. I’ll share the tales of woe (and wonder) as they come. But in the meantime, I decided to write some tips and tricks for all of you on the practice side to help prepare for Meaningful Use.
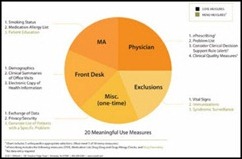
Meaningful Use: 15 Things Your Practice Can (and Should) Do Now
Note: This assumes that the practice and physicians have already decided to try to demonstrate Meaningful Use and have chosen the Medicare path. Most of the folks who are going for the Medicaid path have already figured out they have a much easier road and are laughing all the way to the bank in many states.
1. Get thee to a certified EHR. If you are already on EHR, make sure that you are on a version that the vendor has certified with one of the Meaningful Use certification bodies. Beware of phrases like “certification compliant,” as that is similar to “board eligible.” The Feds require that you be on a certified version — end of story. Pending or compliant doesn’t cut it. If you are not on the certified version, immediately schedule a consultation with your vendor / reseller / technology partners to determine what it will take to get you on a certified version. If you are not already on an HER, are in the search process and achieving Meaningful Use is a significant consideration, you might want to use certification as a litmus test to make your search easier.
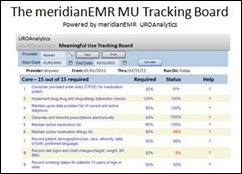
2. Make sure you understand your vendor’s reporting strategy. Are they providing “out of the box” reports that you just have to deploy to see how you are doing? Or do you have to hire a report writer or consultant to get the reports you need? Ideally, you want the reports in hand so you can run them throughout the year and see how you stack up prior to submitting your data.
3. Make sure you understand the HITECH program. Providers need to be intimately familiar with the objectives and measures, whether they think they do or not. They should be able to articulate what is expected of them if they plan to be successful. Failure to show up to meetings where this is discussed or to participate in discussions about changing office workflow are not favorable signs.
4. Register with CMS. If you have never been to the CMS overview page, bookmark it now and visit it often.
5. Determine exactly where and how in the EHR measures need to be documented. I’ve seen several vendors put together MU slide presentations that outline this. For those providers that don’t always pay attention, I recommend printing this, highlighting it, and hanging it at various places throughout the office, preferably where the providers habitually document their visits. There should be no question on where the data should be entered.
6. Understand that MU is not graded on a sliding scale. It’s pass-fail. You either pass all the elements or you do not get your money. There is no partial credit.
7. Ensure the EHR is configured properly for MU. Some systems require certain settings be enabled to support MU documentation. Ensure that your allergy and drug interaction checking is enabled and that providers cannot turn it off. This sounds like a no-brainer, but you’d be surprised at some practices’ system configuration.
8. Read Evan Steele’s HIStalk article, Meaningful Use Does Not Have to Burden Physicians. This should be required reading for practice managers. The vast majority of MU objectives and measures can be achieved by leveraging support staff. Physicians should not be asked to serve as data entry clerks. It’s unfortunate that, all too often, poor workflow design and failure to adequately train staff puts them in this role.
9. Ensure providers are enrolled in electronic prescribing and know how to use it (and when it’s legal to do so). Providers need to be sending more than 40% of permissible prescriptions electronically unless there are certain hardships, like being in a rural area without Internet or having insufficient pharmacy participation. Look carefully at your workflow to make sure that processes, like allowing nurses and other staff to refill medications in some situations, are not going to drive your percentage down.
10. Analyze offices process for collecting demographic information. You need a sensitive plan to collect language, race, and ethnicity data without having to explain to every patient through the front window. I personally like the approach of using a patient data collection form (or use a kiosk if you have one) so the patient can complete this privately. If the patient doesn’t complete it, have a members of the nursing staff ask about it in the exam room. Be sure the system is configured to include the appropriate descriptions and codes – eliminate home-grown or customized descriptions from pick lists NOW.
11. Whether you’re still on paper or fully electronic, update problem lists NOW. Since you are already asking the patient to fill out a demographic update sheet, why not use the opportunity to gather pertinent medical information as well? Too many practices simply ask the patient, “Has anything changed since your last visit?” The yield from that question is not very good. Consider mailing an update to patients prior to an upcoming visit or having them complete a questionnaire via a patient portal or kiosk. When I started doing this annually in my practice, I was shocked at what patients had forgotten to tell me.
12. Update medication and allergy lists NOW. See above. Really, for good patient care you should be doing this every visit. But now, when the patients complain that you are asking them to validate their medication list (and I do hate arguing with the sweet geriatric ladies who say, “But Doctor, I know you know what I’m taking”) you can thank your friends at Medicare for making you do it and make sure the patients know who is behind all the fun their having updating their information.
13. Clean up (or create) office policy and procedure documents regarding patient care elements included in Meaningful Use. Make sure all staff understand (physicians too!) and sign to indicate their understanding. This will be very helpful down the road when folks argue with the IT and management teams about why their data doesn’t show them meeting the criteria. Don’t forget to include vitals, smoking status, quality measures, etc.
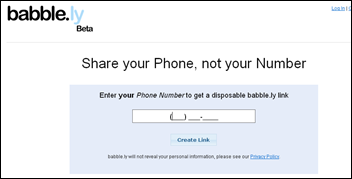
14. Determine your strategy for providing patients with electronic copies of their health information. Are you going to use a Web portal? Burn it to CD? Interface with a personal health record? Give them a jump drive?
15. Prepare to meet technical requirements for data exchange and security. Make sure staff understand what they need to protect patient information and deal with deficiencies promptly.
16. If your office does not have a CMHO, identify one immediately. OK, I couldn’t resist adding one more item. What is a CMHO, you ask? Chief Medical Humor Officer. Because once the practice fully embraces Meaningful Use, there’s going to be a need for humor STAT.
If you’re savvy enough about Meaningful Use to understand most of the items above, you’re probably in a reasonable position to prepare to demonstrate MU. On the other hand, if you feel like you’ve just tried to read a novel in a foreign language, you’re going to need some help. You may want to consider contacting your state’s Regional Extension Center (REC) for assistance. Other good sources include your state Medical Society or various medical specialty organizations.
Have a question about Meaningful Use or the best suppliers for nitrous oxide (laughing gas?) E-mail me.















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…