HIStalk Practice Interviews Eric Morgan, CEO, AdvancedMD
Eric Morgan is president and CEO of AdvancedMD of Draper, UT.

Give me some background on AdvancedMD.
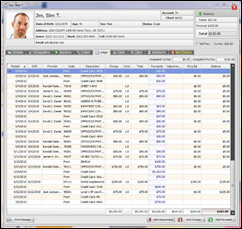
The company started out around 2000. That’s when we first launched our first SaaS product. In 2002, AdvancedMD was formally launched. We brought the practice management solution to market for the small physician market. We were very early on in the going to market with what we would call a pure play Software-as-a-Service offering.
That’s been the way the company was founded and built and has grown and maintained ever since. We pride ourselves on being one of the first — and not only in this industry, but across many others — early adopters to embrace this business model in the marketplace. We believe that is a big factor for why we’ve been so successful.
You acquired PracticeOne just last year.
Yes. We bought PracticeOne in December of 2009. The primary focus for us was to get what we felt was a market-leading EMR product that was CCHIT-certified with additional certification for cardiology and pediatric subspecialties.
Given the move towards Meaningful Use and what we were seeing in the marketplace, we knew we needed to make that move very quickly. Things had accelerated quickly in 2009 since the HITECH act. Our primary focus was getting what we felt was a market-leading EMR. That’s exactly what we’ve done.
It’s a very strong product that is Web-based. PracticeOne, like many vendors and most major vendors, was offering it on both as an on-premise client server as well as a SaaS offering, or ASP as most call it. We have now moved that to a pure SaaS offering and integrated that into our product. That was really what that acquisition was all about for us.
What is the status of the integration of the practice management and EMR products?
We’re ahead of plan on the success we had hoped for. We’ve integrated the product. We spent time to work through that and do it right. We just last month launched that integrated product and we are very excited about where we stand.
We have had a lot of interest in our customer base as well as in the new customer marketplace. We’re finding, every single month, we’re selling more and more EMR products to the marketplace to the point where we are, as I said, ahead of any plans that we had in place when we made the acquisition back in December.
How difficult is it for a privately held companies, whose income statement and balance sheet are not publicly available, to convey a solid financial position?
That’s an important question because it’s one of those areas that we do talk about. Certainly on an individual customer basis, it’s something that we can have a conversation with customers about. Frankly, for most physicians, it just doesn’t come up. While we’re not the biggest company in the industry, we have a substantial critical mass, we’re very strong financially, and it’s not a concern for the buyers in the marketplace.
With that being said, not being a public company has its advantages and certainly things that are helpful. But on the downside, you lose some of that visibility that the public companies get. So for us, we take the approach of sharing more information, rather than less, so people really get a picture of how we’re doing and how strong we are. We think that’s important particularly in this market because we believe, in the next few years or even less, company viability and strength is going to become a much bigger factor for the marketplace and success.
It was OK over the years to buy software from a small shop that may have built a practice management system and had only a handful of customers. We all know there’s a lot of vendors in this marketplace, but going forward with the bar raising significantly with Meaningful Use, ICD-10, 5010, integrated EMRs and practice management, interoperability — all of those factors are raising the bar substantially. We feel the smaller vendors are really going to struggle to keep pace. So, as a private company, it’s important for us to get the message out that we’re strong, growing, and very viable, and that we’re going to be here for the long haul.
Do you see more consolidation in the practice PM/EHR market? And, is that a good or bad thing?
Consolidation is a word that we use a lot. I think the answer is there is going to be a shorter list of vendors that are going to be doing well, and there’s going to continue to be a longer list of vendors that are going to consistently struggle. I believe, yes, consolidation will take a variety of forms. I’m not sure that we’ll see a whole lot of mergers and acquisitions or buying or consolidating of companies, necessarily, because that’s challenging and problematic from a product perspective.
However, I think we’re going to see a lot of the small vendors struggle and look for alternatives. We’ve already seen that in the marketplace. We saw that when we went out to the market and made the purchase for PracticeOne. We looked at a lot of companies and we saw the state that these companies were in. They’re in a very precarious position, in our opinion, in a marketplace that’s in the process of exploding.
Switching gears, your AdvancedBiller partner program aims to compete with companies like athenahealth. Does the software include the same type of rules engines that you have with athenaCollector? Are customers billed based on collections?
The first part of your question is yes, they are. We do have a very robust rules engine and we would argue that it’s as strong, or stronger, than anybody on the marketplace. That’s why we’re able to get over 98% of claims that are submitted go through to the clearinghouse and payer on the first pass, and the rejection rate for our clients is so low.
That is something that we feel is a strength for us. Our customers value it. They tell us that. We don’t think anybody does better than us in terms of delivering on that. I do believe there are vendors in the market who market that better than we do, and to their credit, but in terms of performance, we feel there’s no one that is better than us.
On your second question about pricing based on percentage of collections, we don’t do that ourselves. We do that through our billing service partners who are part of the AdvancedBiller program, which is an industry-leading, unique approach to this marketplace.
No one else that we are aware of has something like it. Instead of competing with the billing service companies that are out there, we are partnering with them and providing the technology and they’re providing the expertise of the billing service offering. They price their offerings, typically, by percentage of collections. That may include our software as part of that. We work out the pricing in a more traditional manner between us and the billers, so that’s a different model.
I’d also like to note that that is an important point because it appears that a lot of folks — as we move more and more to EMRs/EHRs — that they are uncomfortable with having necessarily their billers, like an athena. Also, athena prices their EHR based on a percentage of collections. That does not seem to feel right to a lot of doctors. It’s one thing to do it based on your billing side, but to do it on your clinical side is a little challenging.
The other concern that we’re hearing in the marketplace is the lock-in that goes along with that. It’s one thing to commit to a billing service or an athena knowing that in some time I might transition and bring billing back in-house, but it’s another one once I’m committed to them on my clinical system. Then I’m finding myself in a situation where I’m maybe more locked in.
We’re seeing those two factors really being a disruptive force for some folks in the marketplace.
Do many practices still raise concerns about not having their data stored on a server in their office?
We have a very strong policy that we don’t hold anybody’s data hostage. While there’s a concern and perception about that, the reality of it is that it that really, for the customer, it should look no different than the server sitting in the corner of the office. In fact, the data’s much more secure in our environment than it would be for an office trying to manage backup and recovery of data in their own environment. It comes up and we talk to it, and we’re very successful at getting people comfortable with it.
There’s going to be a certain group of folks who just for whatever reasons can’t get over that and they feel they need to have everything in-house. That’s fine, but we’re finding there’s less and less of those people, and people getting more and more comfortable.
We’re adding nearly 200 new practices every quarter. We expect that to accelerate as we go into the end of 2010 and 2011. Going into next year, we’re looking at 200-250 or more practices signing up for us each and every quarter. I think that gives you an indication of our traction and the acceptance of our offering, both the product and the business model with SaaS.
How many physicians does your typical client have?
We have clients of all sizes, but most of our clients are less than 10. We have many, a very large percentage, that are even less than five. We do focus on the small practice market, by definition. It’s not so much about the product or anything else as it is historically, those tend to be the size of practices that would buy software this way. It’s a viable and attractive offering to them. More and more we’re seeing larger practices willing to do it as well.
The one thing that’s unique about AdvancedMD is that we have been able to successfully offer a solution to the one-, two-, three-doc offices, which has historically been a challenge for vendors to do and do in a way that is economical for both the practice, in providing value, as well as something that is sustainable and profitable for the vendor. The combination of our business model with SaaS and our offering that has allowed us to do that. I think that’s the thing that’s truly unique about AdvancedMD.
The EHR adoption rates for 1-5 doctor practices have been notoriously low. What it will take to increase it?
I think it has been low, and probably for some good reasons and not-so-good reasons. I think what it’s going to take is — despite our challenges of getting our arms around Meaningful Use in the industry — from the perspective of how long it’s taken to get clarification and the complexity; I think now that it’s clear, the market can get comfortable that vendors like AdvancedMD can deliver on that and move forward.
I think what we’re going to see happen is that at some point in time, physicians are going to realize, “I can no longer not be on this.” I call it being off the grid. It’s one thing to resist or say it’s not really important to me now, but when the day comes when a doctor’s not getting the referrals from a primary care physician because they’re not electronic and they’ve got to go back to manual processes, I think the a-ha moment is going to hit them that we won’t need government stimulus anymore because the tipping point will have occurred and that physician will jump on.
It’s like the person back 10-15 years ago who resisted e-mail. Finally, everybody including Grandma got on e-mail, because if not, they couldn’t stay in touch with their grandkids and it became a problem. I think we’re going to have a similar situation where, regardless of where you are in EMR adoption, you’re going to realize one day that you can’t afford not to do it because you’re going to be off the grid. I think that’s the power of Meaningful Use because I call it more of a catalyst than a stimulus.
Given the new ruling on EHR certification, how does this affect your business and your plans to seek certification?
I think it’s just good to get the clarification. You know, we’ve been on top of that all along, like most vendors who are dealing with this. We’ve been very proactive about keeping abreast of where things stand, so I think it’s great that we just have the clarification.
We’ll be ready for our clients to be able to start collecting the stimulus money next year as scheduled. We see that as a double-edged sword. There’s a lot of compliance that needs to be done there, but it’s all the things that matter. It makes a lot of sense if you really look at what they’re asking for. We’re excited to have that clarification and sort of eliminate some of the confusion that has existed in the marketplace over the last year or more.
Have you decided if you will get certified through CCHIT or are you considering other certification bodies?
We haven’t made a final decision on that. We’ll proceed based upon what we think will make the most sense. I think there was some confusion over the last 12 months with comprehensive certifications and so forth, and I think how that plays into ARRA and the Meaningful Use certification.
Clearly in the past few months Meaningful Use carries the day. Whatever it means that we need to do to comply with Meaningful Use, we’re going to do. If that means there are other certifications, we’ll do it. If not, and we feel those aren’t necessary and they’re extraneous, then we’ll make a decision that way. We’re prepared to go either way and we haven’t made all the final decisions, but we’re very focused now on Meaningful Use.
Are hospitals driving more practice EHR decisions? If so, how does that change your strategy?
We’re seeing that as a trend. It’s a little tough because what you see a lot is anecdotal. I think there are some cases where we’ve seen physicians move to the hospitals’ direction or influence.
At the same time, I think we all know independent physicians are called independent for a reason. They tend to not want to be too locked in to any one supplier or to one facility. It’s going to depend on market and rural versus urban and suburban and so forth, so we’re seeing some of that.
I’m certainly seeing some announcements from vendors. It’s not clear to me that those announcements are necessarily carrying a lot of doctor adoption to them, but a press release like that is always nice to have. I think we’re keeping a close eye on that.
We are looking and moving more towards discussions with hospitals and we feel that’s an area to focus on, so we’re certainly not ignoring it. But, again, I’m here to say that 200 practices every quarter are signing up for AdvancedMD, so there are folks that are, in significant numbers, buying directly and not going that route.
How price sensitive are EHR prospects?
You know, interestingly, price has not been an overwhelming issue for us. With our model there’s a low upfront fee, there’s low capital cost, and then it’s a monthly subscription. It’s a very attractive model in the first place. We do our contracts on a month-to-month basis so they can always get out of them, so they’re not locked in.
Price has not been a major factor for us. We certainly have put some incentives out there to get people started, but that’s more us being proactive than it is necessarily huge pressure from the marketplace.
We are strong, strong believers of the value of our offering and, quite frankly, good quality offerings in the marketplace. We believe a strong, integrated practice management EMR system has a tremendous ROI. We believe that that’s the way doctors should buy it, as an integrated solution. What we call medical practice optimization. We are very much believers that the world needs to get away from thinking in terms of modules or areas. This is really an automation of the practice, and the return on investment in both hard dollars and soft savings, we believe, is very strong.
Where do you expect the company to be in three to five years?
We expect AdvancedMD to be among the leaders in the marketplace. We would expect us to be on a very short list of names that would be mentioned in the marketplace when you’re talking about medical practice optimization. And, as one of the companies who grew up in the early days of this cycle and moved through this Meaningful Use and grew and thrived in that marketplace and really separated themselves from others. We would be expected to be on par with any of the big names that you would know of in the marketplace today.














The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…