Putting the “Value” in Value-based Care
By Jim Higgins
Jim Higgins is the CEO and founder of Solutionreach in Lehi, UT.

Healthcare in America has struggled with multiple challenges in recent years. Costs are at an unprecedented high while health outcomes are subpar. As of 2017, the cost of healthcare in the US averaged $10,345 per person — the highest healthcare costs in history. And yet, despite spending twice what other developed nations spend for health care, Americans experience a lower life expectancy, greater prevalence of chronic disease, and overall poorer health outcomes. Walter Cronkite once echoed the thoughts of the general public when he said, “America’s health-care system is neither healthy, caring, nor a system.”
In an effort to make care more convenient, effective, and affordable, the healthcare industry has recently been shifting away from volume-based care towards value-based care. This means providers are increasingly receiving payments based on the value of care they deliver rather than the amount of treatment completed. While the push to make this move has been going on for nearly two decades, it’s only recently that the shift has really picked up steam with both government and commercial payers. Experts note that the trend towards value-based care will continue into the foreseeable future. According to a 2016 survey from ORC International, 58 percent of payers are moving towards full value-based reimbursement, and 63 percent of hospitals were part of some ACO. Those numbers continue to grow about 10 percent each year.
What does value-based care mean?
As with any big change, adopting a value-based care model leaves providers with questions. Many of these questions revolve around the meaning of value. How is value defined? What services constitute value? How can a practice determine if they are providing sufficient value? To understand how to implement value-based care, it is critical to know how value is defined. The following are the key initiatives payers use to determine value in a value-based care payment model.
1. Patient experience. At the center of value-based care is the patient experience. Not to be confused with patient satisfaction (which is a subjective measurement), the patient experience encompasses every interaction that can be easily measured. Measurement is key. The patient experience includes things like ease of scheduling, wait times, patient access to healthcare records, and clear communication between the patient and provider. To provide excellent value, every aspect of the patient experience should be as seamless and easy as possible.
2. Proactive care. A major goal of the value-based care model is to improve poor health outcomes through proactive care. Proactive care includes preventative care as well as on-going care for patients with chronic conditions. In days gone by, proactive care often meant simply outlining a health plan and hoping patients adhered to it. Today, practices are expected to implement specific strategies to actually motivate patients to follow those health instructions and show up for regular appointments. Proactive care starts with uncovering the reasons behind non-adherence and then removing those barriers. This often requires more touch points of communication than many practices have historically given. Proactive care strategies can include everything from appointment reminder texts to educational newsletters to video explanations of treatment to medication reminders and more.
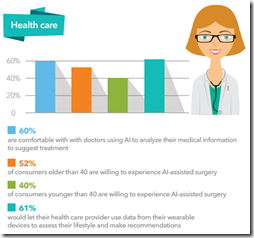
3. Patient risk assessment. Using technology, patient data can be analyzed to identify those who have potential health risks. These are the patients most likely to have poor health outcomes and, subsequently, need proactive care. According to a recent Chilmark Research report, current risk stratification models account for only 10 percent of a patient’s health outcomes and are not sufficient to meet the standards of value-based care. These risk models focus on the needs of the practice rather than the needs of the patient. Value-based healthcare organizations should include social, behavioral, and environmental factors in their risk assessments. These social factors account for as much as 70 percent of health outcomes.
4. Care coordination. One “value” pillar that practices should examine is the effectiveness of care coordination across the entire healthcare system. Care coordination, while important for all patients, is especially critical for those patients deemed to be high risk. When care is coordinated across all specialties, practices are better able to eliminate gaps in treatment. Care coordination requires comprehensive and timely communication between all of a patient’s providers and, when done well, leads to improved care and better health outcomes.
5. Patient-reported outcomes. Using a combination of surveys and questionnaires, patients are being asked about their healthcare experiences more than ever. Patient-reported outcomes are defined by the FDA as "any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else." It is through PROs that the more subjective information about a patient’s experience is gathered. Collecting and evaluating this information provides insights that enables practices to develop a more patient-focused (i.e. value-based) process.
The shift to value-based care is often overwhelming at first, but knowing the basics helps ease the transition. The growing pains are worth it. As practices adopt value-based care, the entire healthcare system will benefit — including providers, patients, payers, and society as a whole. Value-based care reduces costs, increases efficiencies, boosts patient satisfaction, and results in better health outcomes. Dedicating the time and training needed to put the “value” in value-based care is a win-win for everyone.
Contacts
Jenn, Mr. H, Lorre
More news: HIStalk.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.



![]()



















Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…