Tom Check is president and CEO of New York-based Healthix, the largest nonprofit HIE in the US.

Tell me about yourself and the organization.
I’ve been in healthcare IT since 1985. I was in senior IT positions at NYU Medical Center and Mt. Sinai Medical Center here in Manhattan for almost 19 years , so I’ve gotten to know the provider side of the business pretty well. I spent eight years as the CIO at the visiting nurse service of New York, which is the largest not-for-profit home health provider in United States. I gained a better understanding of community-based services and the continuum of care between the acute, post-acute, and sub-acute settings.
I’ve been president and CEO at Healthix for the last four years. We’re the largest HIE in the country, with data of over 16 million people here in New York City and Long Island. Healthix has been around for about eight years now. It started as three separate HIEs – one in Long Island, one in Manhattan and Queens, and one in Brooklyn. Over the last few years, we’ve merged and created a single HIE for New York City and Long Island, and that’s the scale that we’re at today.
How have you seen physician practice participation change since the HIE got its start?
In the early days, it was really the hospitals and a few of the very large nursing homes that were the founders of Healthix and its predecessor organizations. In those days, physician practices got involved when they could take advantage of specific, grant-funded opportunities that a hospital might be pursuing – grants that were really were focused on engaging the players of community-based care. It was really in the context of specific grant initiatives. What’s changed a lot in the landscape and increasingly so in the last few years, is the move toward value-based payment, which really requires understanding and managing patient health and experience on a much more continuous basis before the acute episode, during the acute episode, and after the acute episode. It really requires coordination across all the providers.
Whether it’s a PCP that’s providing care management services, or a care manager, ACO. or health plan, there’s a need to coordinate the care across all those specialties – physician specialties as well as hospital-based specialties. Increasingly, we’re seeing those kind of programs come together. When they do, they identify who their partners are in the community – the physicians that they really need to be part of the HIE.
At this point, nearly all of the FQHCs in our area are very strong participants in Healthix. The largest physician practice groups are very strong and active users of Healthix. In fact, one of the very large physician groups is one that’s constantly monitoring patient healthcare experience – if their patient presents at an emergency department, those physicians can follow up and support that patient whom they’re managing through those experiences.
Increasingly with the federal initiative toward transforming Medicaid to value-based payments, New York State is a participant in the Delivery System Reform Incentive Payment (DSRIP) program, the district program through which they plan to transform Medicaid to a value-based payment system over the course of five years. New York has set up performing provider systems across the state to coordinate the care of Medicaid beneficiaries. Those groups have very large numbers of community physicians that need to be part of the program. They’re encouraging us to bring them in to the Healthix fold so they can be part of the program. I expect we’re going to see more of that. It’s really the move towards more coordinated care and value-based payment that’s bringing physicians more into the ecosystem of HIE.
What are the challenges in signing physician practices on to the HIE?
It has to be a more low overhead kind of decision for a physician practice. They’re very busy and so the implementation has got to be painless. The good news is that there is much more of a presence of EHRs in physician practices now than there was even five years ago. A great many of the physician practices in our area, especially the small practices, are using a hub-based model or cloud-based model EHRs, where they really don’t have to have hardware on their premises; they don’t have a server to maintain because the software company is doing that for them.
We have direct connections with those EHR software companies, so that when the physician authorizes it, they can pretty easily connect the physician using their software to us because the connections are all running through their central hub. That’s really made it easier for us to implement physician practices. It’s made it much less expensive. By the way, Healthix is regulated and funded by the New York State Dept. of health, which means that we don’t need to charge physicians or any other provider for ongoing use of our services, which is a real benefit.
The technical complexity of implementing a connection with a physician practice has gotten much easier over time. The biggest item at this point is to first have a conversation with the physician practice about what the benefit will be to them or what benefit we can provide to them. That benefit is typically giving them connectivity with the other healthcare providers that are in the referral network for their patients. That’s really what we need to present. When we can demonstrate that benefit to a physician, then the implementation is pretty straight forward.
How does an HIE like Healthix, and the larger SHIN-NY network, add value to population health management programs?
By way of overview, the SHIN-NY network consists of eight different HIEs in the state all regulated by the state health department. We collaborate and have a common master patient index. Through that, we know which patient has data in each of the eight HIEs across the state. That means if the provider or anyone of the HIEs queries for a patient’s data, that HIE aggregates it from across the state and brings state-wide results back.
We can alert the physician if the physician wants to be alerted. We can alert them when their patient presents in the emergency department or the hospital, or has some other significant condition. We’re expanding that to be able to alert them if the patient has that kind of event within another HIE, a neighboring HIE, and over time that will expand statewide, too. There are other things that the HIEs are doing to collaborate. The gist of it is to create a virtual patient record that expands the person’s encounters across the state and that allows for a better management.
Analytics is another core area that a lot of HIEs are moving into. What Healthix would like to do is leverage our predictive analytics capabilities along with those risk scores that we assign to patient populations that we follow and do some real-time alerting that could be shared across the network. Our goal is to put the information into the hands of the clinician who’s seeing the patient to make it actionable in real time. We see our fundamental territory and region being New York City and Long Island, but if they’re up at Winchester or Albany … I’m up there visiting as a patient, I end up in the healthcare system. I want to give them the ability to send and exchange information down to Healthix here in the city area in the southern part of the state, as well as the other way around. The predictive analytics, the risk stratification scores, and to some extent, population health can be extended across the different RHIOs here in New York.
Healthix made news earlier this year for implementing a new predictive analytics solutions from HBI Solutions. Why now?
We had already implemented some measure of analytics that was looking at the clinical content of the patient’s experience; in other words, you start with the event that the patient had on ED admission, and then you look at the analytics behind that as to what was the condition, what were the presenting symptoms. The next thing was to get into predictive risk, which is running the analytics against the body of information that accumulated on the patient.
Predictive analytics is one of our big focus areas, and I see it bringing the most value to those small and medium-size organizations that for many reasons either haven’t had the time or don’t have the means to invest in a technology like this. An advantage that Healthix really brings to the table is that we see a lot of information on the patient. I think our number is up past 240 organizations that send and receive data through us today. We really get that holistic view of the patient’s wellbeing from the provider’s viewpoint. Leveraging that as a service, we can offer those organizations the ability to better manage their patient populations. We find ourselves really in a good position to leverage that data to help them on this journey.
Has New York’s shift to mandatory e-prescribing affected HIE utilization in any way?
It has been helpful in a number of ways. First of all, e-prescribing has really encouraged doctors to be on current versions of EHRs. It’s increased the penetration of the EHRs in physician practices. One of the approaches that we take at Healthix is that we really want the doctor the be able to get the information that’s in Healthix through their EHR rather than having to come to our portal.
We’ve really worked with the EHR vendors so that when the doctor is working on patient John Jones in the EHR and the doctor wants to see information from Healthix, they can typically touch a button within the EHR and it reaches out to us and tell us who the doctor is. The doctor’s already been authenticated, so we know who the doctor is, we know that they’re looking at the record of John Jones, we know who John Jones is in our system, and we can bring a CCD back for the EHR to display to the doctor.
We’ve even taken that one step further and given the EHR software the ability to reach out and query, "Does Healthix know about John Jones? Do we have any data about John Jones from other sources? Do we have any data on John Jones from those other sources since the last time the doctor looked up his record in Healthix?"
Finally, New York requires that the patient has to give consent for the provider to view the patient’s data. It looks and sees it has consent from John Jones for the physician practice to view his data. Given all that, it comes back in the background without the doctor having to ask for it. It comes back with an indicator – green light, yellow light, or red light – that the EHR will display.
Green light would mean you’ve got the patient’s consent, Healthix has data from other sources, and it’s data you haven’t seen yet. That really encourages the doctor to click and see what’s in Healthix. It could be a yellow light, which means Healthix has data and you haven’t seen it yet, but you don’t have the patient’s consent. That would encourage the doctor to ask the patient for consent so that the doctor can then see the data.
It may come back with a red light, which says either Healthix doesn’t really have any information other than your own information about this patient, or the information Healthix has you’ve already seen so that the doctor knows not to go through looking at Healthix. That idea of embedding as much access to Healthix as you can right into the doctor’s EHR goes along with initiatives like e-prescribing that are encouraging doctors to use their EHRs more interactively.
Another things that we’re working with EHR vendors on is giving them the ability to easily receive messaging that we may send the doctor. If the doctor wants to be notified when their patient presents in a emergency department or has a change in lab values, we want to be able to send that message to the EHR so that the EHR can easily delivery it to doctor’s workflow – then it fits right into the way the doctor is using the EHR. E-prescribing itself hasn’t had as much a direct impact as the whole set of initiatives that are encouraging physicians and supporting physicians in using EHRs.
Could we soon see New York physicians opt in to real-time alerts as Vermont is attempting to do with PatientPing?
I’m not as familiar with what Vermont is doing with PatientPing, but we do have very high utilization of alerts. Of the 16 million patients in Healthix, 2.6 million of those have given consent for their provider to see their records. Of those, 1.3 million patients have subscribed to real-time alerts. Increasingly, we’re growing into giving alerts when clinical conditions change or we will be giving alerts when perspective risk changes.
We currently send out 115,000 alerts every month to physicians and care managers that subscribe to them. We also send out 247,000 CCDs a month for those care managers and physicians that have asked to receive them when certain patient conditions change. We’re already allowing providers to get alerts from us, and by doing things like predictive analytics, we’re hoping that we can tune those alerts so that they really represent alerts when the most significant changes are happening to a patient, where the physician may really want to intervene.
Do you have any final thoughts?
I think you’ve really asked a good set and it really speaks to the value proposition for physicians.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.















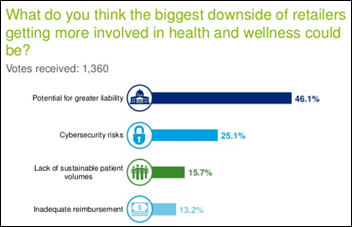












Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…