News 9/17/15
Top News

Echoing the Senate HELP Committee’s most recent call to delay Stage 3 of Meaningful Use, the AMA and 41 other medical societies write to HHS and the Office of Management and Budget, strongly urging them to pause the final stages of the Meaningful Use program in light of major changes to Medicare. “There is growing bipartisan recognition in Congress that the direction of the Meaningful Use program needs to be reassessed in light of usability and interoperability challenges with electronic health record systems,” says AMA President Steven J. Stack, MD. “Poorly performing systems that do not facilitate the seamless exchange of data would severely undermine the ability of the health system to support the implementation of the payment reforms outlined in MACRA. Pausing to reassess Stage 3 rules will not stop or delay progress with EHRs,” said Dr. Stack. “On the contrary, we firmly believe a temporary period of reevaluation will help move the program forward and drive innovation and adoption.”
HIStalk Practice Announcements and Requests
There are just a few days left to take advantage of special rates on HIStalk Practice sponsorships (HIStalk sponsors get an extra discount) to make sure your message stands out. Contact Lorre for details.
Webinars


September 22 (Tuesday) noon ET. “Just Step on the Scale: Measure Ongoing EHR Success and Focus Improvements Using Simple but Predictive Adoption Metrics.” Sponsored by The Breakaway Group. Presenters: Heather Haugen, PhD, CEO and managing director, The Breakaway Group; Gene Thomas, VP/CIO, Memorial Hospital at Gulfport. Simple performance metrics such as those measuring end-user proficiency and clinical leadership engagement can accurately assess EHR adoption. This presentation will describe how Memorial Hospital at Gulfport used an EHR adoption assessment to quickly target priorities in gaining value from its large Cerner implementation, with real-life results proving the need for a disciplined approach to set and measure key success factors. Commit to taking that scary first step and step onto the scale, knowing that it will get measurably better every day.


September 22 (Tuesday) 5 p.m. ET. “Laying the Groundwork for an Effective CDS Strategy: Prepare for CMS’s Mandate for Advanced Imaging, Reduce Costs, and Improve Care.” Sponsored by Stanson Health. Presenters: Scott Weingarten, MD, MPH, SVP and chief clinical transformation officer, Cedars-Sinai; Anne Wellington, VP of informatics, Stanson Health. Medicare will soon penalize physicians in specific settings who do not certify that they consulted "appropriate use" criteria before ordering advanced imaging services such as CT, MRI, nuclear medicine, and PET. This webinar will provide an overview of how this critical payment change is evolving, how it will likely be expanded, and how to begin preparations now. A key part of the CMS proposal is clinical decision support, which will help meet the new requirements while immediately unlocking EHR return on investment. Cedars-Sinai will discuss how they decreased inappropriate utilization of diagnostic tests and treatments, including imaging.
#HIStalking Tweet Chat

Frank Fortner (@iatricFJF) will host the next #HIStalking tweet chat on Thursday, September 24 at 1pm ET. Stay tuned for discussion topics. Check out past chat recaps here.
Announcements and Implementations
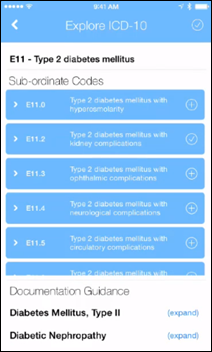
AHIMA adds expanded mobile capabilities to its Clinical Documentation for ICD-10 by Specialty: Principles and Practice app, developed with ImplementHIT. New features include an additional Evaluation and Management Coding library, targeted notifications tied to corresponding training modules, and the ability to build and distribute custom content.
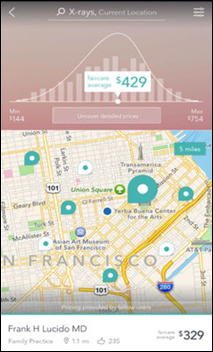
San Francisco-based FairCare launches an iOS version of its healthcare price transparency app.
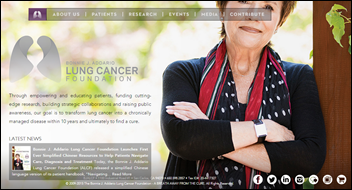
The Bonnie J. Addario Lung Cancer Foundation launches the ALCF Patient Portal as an interactive, educational resource for patients and caregivers.
Telemedicine

Atlanta-based MyIdealDoctor joins the CommonWell Health Alliance, making it the first telemedicine-focused company to join the organization. Additional new members include Varian Medical Systems and Beyond Lucid Technologies.
Authentidate partners with Aeon Clinical Laboratories to offer a genetic cancer test with telemedicine-based genetic counseling for prescribing physicians. The test, which looks at 38 genes, is designed to identify increased risk of colorectal, breast, pancreatic, ovarian, gastric, melanoma, and stomach.
People

Jason Adams (West Central Behavioral Health) joins Medytox Solutions – parent company of Medical Mime and Medical Billing Choices – as CFO.
Patrick Kennedy (PJ Consulting) joins RemitData’s Board of Directors.
Acquisitions, Funding, Business, and Stock

VillageMD secures a $36 million Series A financing round led by Oak HC/FT. Ann Lamont, managing partner of Oak HC/FT, will join VillageMD’s Board of Directors. The Chicago-based company, which assists physicians in transitioning to a value-based business model driven by primary care, plans to use the funding to expand beyond the markets it serves in Texas and Indiana. (I interviewed VillageMD co-founder Clive Fields, MD earlier this month.)
Government and Politics
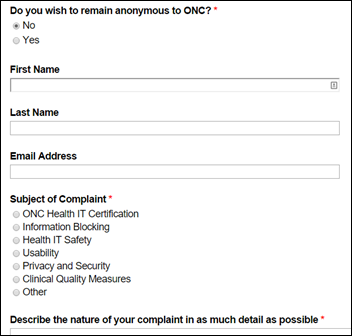
ONC’s EHR complaint form goes live (no joke).
Research and Innovation

An AMGA survey reveals that multi-specialty medical groups and integrated delivery systems anticipate fee-for-service payments will decline by 24 percent over the next two years – not a huge vote of confidence for government and industry attempts to shift to value-based care. Major impediments to a quicker shift include inadequate access to administrative claims data; poor data transparency and data-exchange processes; and a lack of attribution, benchmarking, and risk-adjustment methods.
The Office of Naval Research and Charles River Analytics develop the Mobile, Virtual Enhancements for Rehabilitation (MOVER) system to help veterans recover from brain injuries through virtual coaching. When installed on a Webcam-equipped computer, the MOVER software creates a virtual “skeleton” of the user, which mimics the person’s movements throughout each therapy exercise and offers corrective feedback. The software can also be displayed on televisions via Microsoft’s Kinect gaming system.
An IMS Institute for Health Informatics study finds that there are now over 165,000 smartphone apps geared to health and wellness, yet just 36 make up nearly half of all downloads. The most popular include MyFitnessPal’s Calorie Counter and Endomondo’s fitness tracker. Robert Wergin, MD a practicing family physician and president of AAFP, won’t start recommending apps to patients until he sees more evidence-based research to back up their healthcare claims. “But I think there’s great potential,” he adds.
Other
The local news asks, “Who wouldn’t want a job that pays over $100,000 a year?” in its report on the big bucks associated with working in medical group practice management. The market for group practice management jobs is expected to grow by 23 percent over the next five years. Salaries in the triple digits sound like great opportunities, but I wonder if the job’s stress level is on par with its compensation.
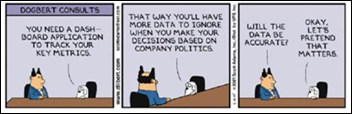
Dilbert puts a humorous spin on data and dashboards. Thanks to @spencerhamons for sharing.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.



















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…