Mansoor Khan is CEO of Persivia.

Tell me about yourself and your background in analytics.
In the late nineties, I had a company called Key Commerce, which developed software in the supply chain space. I’ve always been somewhat entrepreneurial, and that was the first big effort that I made. Key Commerce’s business changed significantly after 911, and so we decided to change directions. My wife Fauzia was getting ready to publish a textbook called “A Guide to Diagnostic Testing,” which included hundreds of algorithms drawn out in a traditional flowchart format. You could take your patient’s history, look through those algorithms and say, “This is where I am now,” and it would tell you what you ought to do next. When I saw that textbook in the early 2000s, my first thought was, this is nice, but it really needs to be in electronic form so that it can be injected into the clinical workflow without requiring the provider to go look up this information.
That was the genesis of DiagnosisOne. The concept behind it was that this would be a system built to help providers create a safety net under them so that they could ensure that at least a minimum standard of care was being met, and it would do so in a completely non-invasive manner. We developed a Web service that sits above watching the clinical workflow. Whenever it identifies a clinical event of interest, it will then take certain actions, such as injecting evidence-based knowledge into the clinical workflow. That’s where we started from. Unfortunately, for the first few years, the data that was available was very sparse and very, very dirty. It was really hard to get the kind of data that you could use to activate or trigger the bodies of knowledge that we had embedded in the system. We kept at it though, and then with Meaningful Use, it jumped up one level in its priority and the provider’s mind set. That priority kept moving up stream as the last five years of Meaningful Use have passed.
Our model was based on enabling EHRs to deliver our knowledge into the workflow. We would sell to the EHR vendor, they would embed it, and they would then resell it as part of their platform or make it available as part of their platform. Our biggest customer was Allscripts, and we had a number of EHRs all the way down to some fairly small ones like Polaris, which is no longer in business.
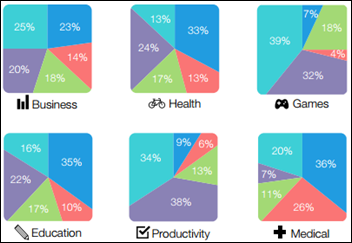
That’s where our interest in analytics came from. We started developing reports, charts, and graphs and then got into the business of reporting on quality measures. That’s what happened till 2010, at which point we raised our first round of funding with Edison Ventures, which allowed us to accelerate the business. Alere approached us two years later in 2012 and bought the entire company.
What was the relationship with Alere like?
We had an excellent relationship with the senior management team, as well as the other divisions of Alere. When Alere acquired DiagnosisOne, our analytics technology was well aligned with the company’s vision for creating a Connected Health platform. Alere wanted to do some really grand things with this new platform, such as working with the UK’s National Health Services (NHS) to take on chronically ill patients and help manage that significant population. However, in 2013, a private equity fund came in and started buying up shares of Alere with the thesis that the company was better suited to stick with its core expertise in rapid diagnostics and sell off the other divisions. The board decided to execute on this plan and they started selling off or shutting down the different assets.
What made you decide to stick with analytics and startups?
Obviously at that point we had a choice. I personally had a choice to take a few months off or do something new. As I thought of taking a few months off, it took me about half an hour to say, okay, I’m bored, now what do I do? My wife and I started thinking what the next evolution of analytics would be. We realized that this is all going to become a game of risk stratification. The ones who can develop really sophisticated risk stratification strategies so they can figure out how to deliver care to the highest risk patients, and how to apportion that care so that the right amount of care goes into each layer of risk … those people will be the ones that are going to succeed in this game.
From there, we launched into the precision medicine concept. Lucky for us that President Obama started talking about precision medicine at the same time, though his concept was a little bit different. When we say precision medicine, we’re talking more generally than that. If you look at diabetes, for example, it is essentially not just one disease. We’re where we were with cancer many years ago, when people thought cancer was one disease, and now we know that it’s literally hundreds of different diseases. Diabetes has a similar profile in that there are many different problems that a person can have. How do you deal with that? One way is to introduce genetic data. While genetic data for diabetics is not really available, we believe that incorporating that sort of data into the systems that are used to manage these patients will allow us and providers to really start bearing down on what sort of treatments need to be delivered to which specific subset of patients. Factor in the introduction of behavioral and consumer social data, and other types of data that become available, then you can really start to develop treatments. And by treatments I don’t just mean medication; I mean a holistic way of looking at the patient to try to impact not just the medication but their lifestyle, their eating habits, their social habits, all of those things that make up the set of circumstances which are going to make you either better or worse in whatever condition you have. That’s been our journey so far.
When you saw the writing on the wall at Alere, did you reach an agreement to purchase the assets of the analytics business as part of your departure?
It wasn’t quite that orderly. Alere was looking to dispose of the those assets, but there are customers that still rely on those solutions. You can’t just shut them down. Alere’s not an irresponsible company, and they don’t want to do something that may cause financial problems for their/our customers, let alone injury or care problems for patients. At that point, we approached them and bought the entire company. We bought the whole thing as a running concern. The employees are still there. The customers are still there. The systems are still there. Because we already had the vision and knew what everything meant, there wasn’t much due diligence that had to be done. The deal could be done very quickly, which was Alere’s big incentive to give it to us rather than to find some third party. Another company would have taken three months to do a deal that we could do in three weeks.
Are you going to rebrand the Alere Analytics assets?
Alere Analytics is going to go away and Persivia will be the only entity that’s left. There will be a certain amount of rebranding. The capabilities that are in analytics actually fit very well with the overall vision that we have with Persivia, and it gives us a set of customers and patients that’s a natural stepping stone for the next set of capabilities that we are now working on. As we deploy those, we’ll have an established customer base with which we can do alphas and betas and start rolling out these capabilities. It will be a very useful transaction for us. We’re not starting from zero again.
How do you feel population health management and precision medicine intersect?
The name of the game in carrying risk will be the ability to stratify your patients into much finer strata combined with very targeted treatment and care protocols. The new risk-stratification strategies being developed now, by companies like Persivia, will allow for a smooth transition from the present day to increasingly higher precision medicine, and eventually to fully personalized medicine, or personomics. We are already ahead of the curve in bringing genomics and personomics to point-of-care, and the new tools we are developing will make this a reality for the care provider.
How do the physicians you work with think about incorporating healthcare IT into their population health and precision medicine efforts? Is this something they’re just beginning to think about?
Frankly, our health system still views population health at a very rudimentary level. Almost all providers, if they have a system, have a claims-based system that does not even take 99 percent of clinical data into account, let alone precision medicine. So we as an industry have to do a lot of work to do in educating and working with clinicians on how these new technologies can be deployed in an effective and meaningful manner.
What’s it like working with your wife? Fauzia Khan, MD was CMO at DiagnosisOne, and COO at Alere Analytics.
I was wondering how to answer that question. That’s got disaster written all over it. The partnership has been good. We’ve been working together now since 2005. She was working at Beth Israel hospital, and she decided to leave that and come work with us full time. As somebody once said, it’s like any other successful marriage – as long as she lets me think I’m in charge, everything goes smoothly.
I think one of the key things is that we are actually very good friends, so it’s not just a marriage, but an excellent friendship, too. We’ve been married about 23 years now. We are quite complementary. I have the IT ad finance background and she has the medical background. She’s very much a people person, so she’s the COO of Persivia and loves spending time with the team. Those are not my strongpoints. I’m much better at talking to customers, dealing with investors, lawyers … all those sorts of things. The division of duties and responsibilities comes quite naturally to us.
The downside, of course, is that work starts at 7:00 a.m. and doesn’t end until 1:00 a.m. It’s always there. Thank goodness we’re both very entrepreneurial. She is probably more of an entrepreneur than I am. We love it and it’s worked out well for us. Our kids also have grown up in this atmosphere. They tend to be very entrepreneurial.
What will the next five years bring for the company?
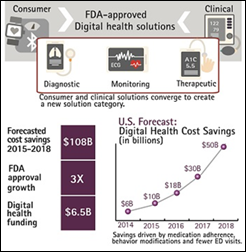
It’s going to be really exciting. As this world of precision medicine and big data merge, the ability to get patients to do the things that they ought to be doing is going to be where there’s tremendous focus and, I’m hoping, advances. I see two areas where there are really big changes occurring. On the provider side are tools related to new disease management protocols and programs that rely on much, much more sophisticated risk stratification strategies. On the patient side are tools that can take all of the different data that’s available about a given patient and identify the areas where you can have the biggest impact on that patient’s health. I think those are the two areas over the next five years that are going to be very, very impactful to our healthcare system, and that’s exactly where we are going to be focused. That’s where we’re going to be investing our capabilities and our resources over the next five years.
Do you have any final thoughts?
Our aim is to empower the patient to take much better care of themselves under the supervision of their provider. We’re looking to create new pathways and new tools that allow them to communicate with each other – truly communicate with each other in ways that have significant impact on the patient’s ability and, more importantly, their desire to do the things that improve their health. That would be my parting thought.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.























The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…