News 8/3/10
Interesting data point: private physicians choosing to participate in the Nebraska Health Information Initiative (NeHII) pay about $20 a month to view the database. For $52 a month, they can add e-prescribing. Sounds reasonable.
Tech Data Corporation becomes the latest distributor to offer Greenway Medical’s PrimeSuite solution. Tech Data will make the solution available to its network of thousands of IT resellers nationwide and Greenway will provide the implementation and ongoing support.
EyeHealth Northwest (OR) signs up for NextGen’s EHR and PM for its 11 offices and 30 providers. NextGen says its recently added 18 other ophthalmology clients and now has about 5,000 ophthalmologists and 500 ophthalmology practices using its software. By the way, here are Q1 numbers from NextGen parent Quality Systems: revenue up 24%, EPS $0.42 vs. $0.36, missing on consensus earnings.
The Kansas Academy of Family Physicians collaborates with Welch Allyn to offer its 1,500 members access to Welch Allyn’s EHR Preparation and Selection program. In addition to access to online tools, members will be eligible for special pricing on professional services from Welch-Allyn.
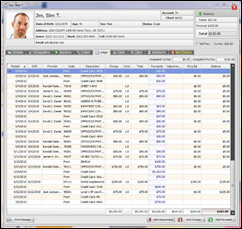
And if you’re in need of a new practice management system, the AMA and MGMA are offering a new online tool kit entitled, “Selecting a Practice Management System.” I wanted to check it out, but looks like both organizations have it in members-only sections . PM vendors can apply for inclusion in the online directory.
To your right: a link to FierceEMR. Mr. H and the Fierce Folks are testing the waters to see if trading links attracts one another’s readers. I like several of the Fierce publications, so take a look if it suits your fancy.
Oncologists will soon have access to evidence-based treatment guidelines at the point of care, thanks to a new partnership with the National Comprehensive Cancer Network and decision support vendor Proventys. The Web-based Proventys CDS Oncology automates the NCCN clinical practice guidelines within clinical workflows.
AirStrip Technologies receives FDA clearance to market its Remote Patient Monitoring solution, including RPM Critical Care and RPM Cardiology. The products allow providers to see vital signs, waveform data, and other clinical information from their smart phones.
While speaking before the House Energy and Commerce Committee’s Subcommittee on Health, AAFP President-Elect Roland Goertz, MD speaks in favor of HITECH grants and technical support for small and rural practices implementing health IT systems. Goertz also asked the committee not to make additional requests of physicians while in the midst of this EHR transition period and asked legislators to consider delaying the required adoption of ICD-10. Bet we’ll be seeing more leaders come forward to ask for an extension of the ICD-10 deadline.
Twenty-one Albany, NY-area pediatric and family practice groups are selected to share a $1 million investment in CDPHP’s medical home initiative. The physician-owned health plan CDPHP picked grant recipients based on their demonstrated their use of EMR and e-prescribing, as well as practice leadership and culture.
athenahealth, iSALUS Healthcare, and MDLand are selected as the preferred vendors for the Indiana Health Information Technology Extension Center (I-HITEC).
This survey suggests that 94% of physicians use smart phones, a figure I find hard to believe. However, there is no arguing that physician smart phone use is on the rise: the same group estimated 59% of physicians used smart phones about four years ago. My phone of choice (the iPhone) was preferred by 44% of the doctors, while 25% liked the BlackBerrry. Not surprisingly, most physicians say they are overwhelmed by the daily volume of communications received by colleagues and patients. I feel their pain.











The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…