An HIT Moment with ... is a quick interview with someone we find interesting. Jon Phillips is managing director of Healthcare Growth Partners, LLC of Chicago, IL.

What economic and market conditions have most affected vendors in the past year and how does the next 12 months look?
Fundamentally, vendors are indirect victims of the challenges facing their customers. Hospitals have seen access to capital disappear, operating results worsen (due to reductions in elective volumes and increases in Medicaid and self-pay/uninsured visits) and dramatic declines in investment income (which helps to fund operations).
Physicians are seeing operating pressures as well, not to mention the indirect impact of declines in value of real estate and other investments and the effect that has on their ability and willingness to spend. Insurers and suppliers remain profitable, but have become quite cautious as the healthcare reform debate works its way through Washington.
As a result of this pressure on customers, vendors are feeling significant stress related to their financial performance. The capital markets see it differently — HCIT valuations are at or near all-time highs as public investors assume that ARRA-related stimulus spending will drive billions in revenue to vendors in the space. At some point, the capital markets expectations will have to meet the reality of customer spending, or customer spending will have to dramatically accelerate to meet capital markets expectations.
The good news is that we are hearing customer purchasing trends are starting to look up, particularly on the physician side of things. However, given the fact that ARRA actually froze much of the market this year as purchasers have been waiting for clarity, our sense is that there is still a long way to go for vendors to feel that they can achieve strong sales growth.
Spending will likely improve across the board in 2010 with solutions demonstrating clear ROI leading the way. Physician sales of EMRs and related capabilities will continue to be strong as practices position for stimulus benefits. Hospital solutions, payer solutions, and supplier solutions are likely to see cautious growth next year as the implications of any healthcare reform package are weighed with regard to how the new environment will impact IT requirements.
We still see strong interest in “pay as you go” models, providing opportunities for providers to acquire systems capabilities while managing upfront capital outlays. While those types of models seem to be spurring sales, many vendors struggle when making the shift to that type of a model since, absent some type of third-party financing, the “pay as you go” model can wreak havoc on the balance sheet of a company used to selling perpetual licenses.
What will drive the M&A market this year?
The M&A market for the balance of this year and into next will be driven by two main trends. First, you will see an increase in the number of distressed transactions. We look at distressed transactions as ones in which the seller is effectively forced to consummate a transaction, generally due to liquidity (i.e. the company is running out of cash).
We expected the distressed market to pick up sooner than it has, but a number of factors have impacted that part of the M&A market. First, with the potential stimulus spending hanging out there, investors have been willing to continue to fund companies operating at a loss in hopes that revenues will pick up and profitability will be achieved in the near term. Unfortunately for many of those companies, revenue growth will recover, but too slowly for them to reach profitability in a reasonable period.
Second, many companies aggressively cut costs late last year and early this year to extend their financial runway. There is not a lot more “fat” for them to be able to take out of their businesses. The result of these two factors is that a number of companies will likely be at or near the end of their financial runway over the next six months. The closer a business gets to that point, the less leverage it will have in its sale negotiations. As a result, we expect distressed deal volume to pick up.
The second main trend relates to investor expectations versus reality. Because of all of the hype surrounding the stimulus spending on HCIT, healthcare IT stocks have rallied, in many cases to their all-time highs. However, if you look at the results being delivered to date (we’ll see if Q3 continues the trend), revenues have been soft, and earnings improvements have been driven by expense reductions. From our perspective, there is a gap between what the markets expect healthcare IT companies to deliver in revenue growth and what they can deliver organically in the short and mid term.
All of the stimulus talk has actually extended sales cycles, and even as the purchasing environment improves, it will take time for bookings to translate into revenue. Therefore, you will see public and larger private HCIT companies looking to acquisitions to augment their internal growth rates.
What companies need to be bought and which companies need to buy someone?
As we mention above, larger companies facing the reality of their sales efforts will need to buy revenue to augment their organic growth. These targets will most likely fall into two categories — share buys and technology buys. Share buys are situations where the acquirer cares little about the target’s capabilities. They are primarily interested in their customers and the opportunity to either up-sell or cross-sell those customers new solutions. Technology buys are intended to broaden an acquirer’s capabilities, using the acquirer’s distribution reach to push a strong product out to a broader customer base.
In terms of companies needing to be bought, if a business has less than six months’ cash on hand, they should be aggressively pursuing an exit, whatever products and solutions they offer. Often we see businesses waiting, hoping that they will be able to raise money or that the market will quickly improve. When those hopes fail, the outcome is generally far worse for employees, shareholders, and customers than it would have been if the business had elected to pursue an orderly exit process rather than an accelerated distressed sale.
If you were launching or buying a start-up, what niche would you go after?
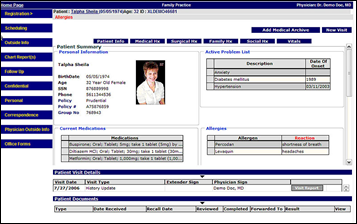
We’d go after a “lowest common denominator” physician-focused EMR that qualifies for meaningful use and that is seamlessly integrated into a physician’s workflow. This type of a solution would likely be a hybrid offering, providing for electronic documentation and order entry but doing it in a way (perhaps with scanning or e-forms) that works with existing clinician workflow. The solution would be priced very aggressively on a subscription basis and would be offered as a Web-based service. We think that a simple offering like this would have the chance to revolutionize the market by being rapidly adopted by small physician groups.
What kinds of vendors will benefit most from stimulus money, both in the short and long term?
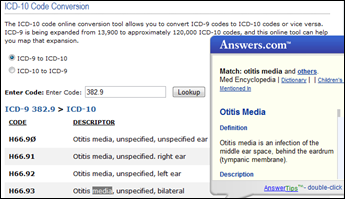
Depending on how meaningful use is defined, vendors most likely to benefit are those that help providers qualify for incentives at the lowest cost. We also see incumbent HIT vendors in hospitals benefitting as they can help shape hospital spending to hit compliance levels.
The other group that is definitely seeing growth is the consulting side of the business- it seems that many organizations are looking to consultants to help them plan their approach to become meaningful users. Those consultants are likely to continue to benefit as organizations implement the solutions that they recommend. However, most vendors probably won’t benefit quite as much as the markets think — “up to $19B” and “incentives” doesn’t mean that the proceeds go directly to HCIT, it just means that providers are rewarded for utilizing HCIT. There’s a big difference.
It is also important to remember that the government gives and the government can take away. We are highly skeptical of business plans built on the basis of attracting stimulus money. It is important to remember that fundamentally the stimulus incentives are being paid to encourage providers to do something that nearly everyone agrees is in the best interest of the healthcare system. As unlikely and unfair as it might seem, it would not be out of the realm of possibility to imagine a scenario where incentive payments are drastically reduced to help cover some other government shortfall.










The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…