News 4/7/11
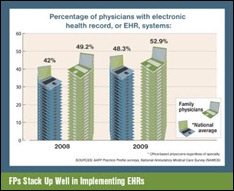
Less than 14% of practices with EHRs believe they meet all 15 core criteria to receive incentive payments, according to MGMA’s 2011 EHR study. Other key findings:
- The main barrier for EMR adoption is expected productivity loss.
- 29% of the 4,588 respondents say they are selecting an EHR.
- Of practices that had adopted EHR, productivity reportedly increased for 27%, decreased for 31%, and stayed the same for 43%.
athenahealth is named a supported EHR vendor by HealthInfoNet, the organization that operates the Maine REC.
e-MDs is named an EHR vendor partner by the Medical Society of the State of New York. Five other EHR vendors were also selected, though I could not find details on the MSSNY Website.
Nuesoft introduces a nine-minute video that provides a high-level overview of Meaningful Use, including how to find certified products, how to apply for funds, and the role of RECs.
Practice Fusion closes $23 million in Series B financing, bringing the company’s total funding to $30 million. This round was led by Founders Fund, an initial investor in Facebook whose managing partner is PayPal founder Peter Thiel. CEO Ryan Howard says the cash infusion will help the company “reach every doctor and practice in the country in our market.”
EMR vendor GloStream will add up to 40 jobs this year and will invest $1.4 million in expanded operations.
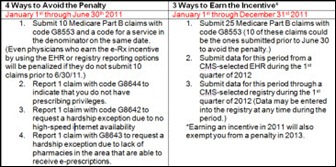
AAFP publishes a resource to help physicians understand how they can earn an e-prescribing incentive from CMS and avoid penalties. The guide includes an explanation of the code G8553, denominator codes, qualified e-prescribing systems, and program exemptions.
Navicure and the American Academy of Professional Coders form a partnership to develop educational resources to help practices practices transition to the HIPAA 5010 standard and ICD-10 code set. Some of the initiatives include a dedicated Website (www.icd10hub.com), regional dinners around the country, and, a Webinar series.
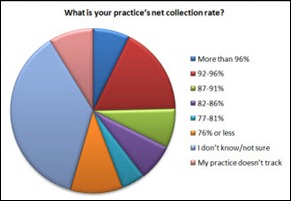
In a random sample that included both clients and non-clients, Kareo finds that practices’ top concerns are reductions in Medicare payments and patient payment collections. The average days in A/R was less than 40 days for 39% of the respondents and only 17% reported a net collection rate of 92-96%.
Phreesia introduces an autism screening tool for its patient check-in technology. Using the PhreesiaPad, parents are able to complete an automated version of the M-CHAT screening tool for assessing the risk for autism spectrum disorder in toddlers.
Please join me in welcoming Capario as HIStalk Practice’s newest Gold sponsor. Capario offers a revenue cycle portal that works with existing PM and billing systems and provides a validation engine that gets claims paid on the first payer submission 90% of the time. The company was named the highest rated indirect clearinghouse in KLAS’s 2010 ambulatory clearinghouse report and processes almost one million transactions a day. The Santa Ana, CA-based Capario offers a dashboard view of the revenue cycle and provides a number of analytics tools to improve cash flow. Capario works directly with providers, as well as with a number of partner vendors. We ran an HIT Moment with CEO Jim Riley a few weeks ago, who offered practical information about RCM vendors, 5010, and ICD-10. Capario is also sponsoring HIStalk, so a double thank you to them!
Sutter Health (CA) announces its $50 million Sutter Community Connect program to provide Epic EMR to qualified independent physicians. Sutter will subsidize up to 85% of the EMR software and implementation costs for physicians in over 100 Northern California communities.













The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…