News 3/29/11
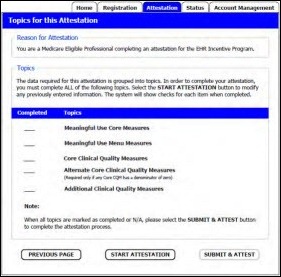
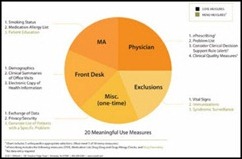
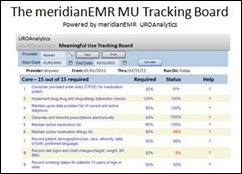
Mark your calendars: attestation for the Medicare EHR program begins April 18th. If you are an eligible provider, you must have an active NPI and have a National Plan and Enumeration System Web access user account. This CMS link includes step-by-step instructions, including screen shots. To date, CMS has paid out almost $37.6 million in EHR incentives and registered 25,217 eligible physicians and hospitals.
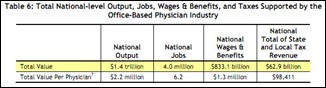
The average office-based physician supported $1.3 million in wages and benefits in 2009, according to an AMA report. Collectively, the nation’s 639,000 office-based physicians supported 4 million jobs and $1.4 trillion in economic activity. That’s about 6.2 jobs per physician.
Pulse Systems names family practice physician Tana Goering, MD as its chief medical officer. Pulse also announces that Loudoun Medical Group (VA) will implement Pulse Complete EHR for 170 of its physicians.
More than 40% of primary care physicians are considering leaving their field, though 60% said they enjoy better job satisfaction than they anticipated on their first day of medical school.
Patients taking advantage of $4 generic prescriptions unwittingly hurt the cause of e-prescribing and EMRs because of the way the transactions are processed and paid for. Patients typically pay cash for these discounted prescriptions, so transactions are not shared with pharmacy benefit managers. As a result, health systems are less likely to receive notification for inclusion in patients’ EMRs. The authors of a NEJM report suggest collecting data from pharmacy records in additional to those from PBMs.
The Wall Street Journal profiles Atrius Health, a Newton, MA-based alliance of five medical groups representing over 800 physicians and about 700,000 patients. Their ACO-like setup has helped reduce costs to the tune of $62 million in 2010. Its collaborative efforts have also boosted quality measures, such as the number of patients receiving cholesterol screening. EMR has played a big role in measuring quality and identifying problems with patient care, as have the use of case managers to monitor chronic conditions and pharmacists to identify problematic drug interactions or cheaper medication alternatives. Still, University of VA professor Jeff Goldsmith notes that not all medical groups and small organizations will have the financial resources to invest in IT and other required improvements: "The idea that this could scale to the rest of the health system is seriously flawed.”
PCIS Gold to will integrate Alpha II’s ClaimStaker software into its medical practice management software.
I mentioned last week that Rhode Island lawmakers were considering a (silly) bill that would ban handwritten medical records. Rhode Island legislators are now considering a seemingly simple proposal reminiscent of my Economics 101 class. The state is struggling to attract physicians, so lawmakers have suggested that commercial insurance carriers be required to pay a minimum of 125% of Medicare fees. In exchange, doctors must participate in the state’s Medicaid program and devote at least 5% of their work to free care. The state medical society opposes the law, fearing the floors may one day become the ceiling.
Meanwhile in Texas, a state representative proposes legislation allowing providers to opt out of a program that requires them to submit patient information to the state. The information collected by the Texas Health Care Information Collection is potentially sold to third parties for market research or health studies. Representative Susan King says the requirement places an unfunded burden on providers and that the state should not be in the business of collecting and selling information without patients’ knowledge.
EyePrescribe.com partners with DrFirst to offer e-prescribing services via the EyePrescribe.com web portal.
NoteSwift names Nuance reseller 1450, Inc. its exclusive distributor for EHR/EMR-related program. NoteSwift works with Dragon Medical to recognize meaningful data in dictations. NoteSwift then inserts the selected data into a provider’s EHR. NoteSwift only supports Allscripts Professional EHR versions 7, 8, and 9.0, though additional EHRs are in the works.
I usually defer to Mr. H when it comes to harsh criticism. However, after reading this article, I decided I can no longer remain Ms. NiceGirl. A local paper details the struggles of physicians adopting EMRs, yet the journalist clearly doesn’t have a handle on the industry. For example, the article says that EMR software “can range from free to over $800,000.” I’m not sure why $800,000 is the magic number since the price tag can definitely go higher for larger groups. eClinicalWorks software is labeled as “chronic disease management-focused” and “super-specialized,” as opposed to NextGen, which can “cater to almost any need.” Huh? And, I have no idea what this is suppose to mean: “The (Epic) software speaks multiple languages to enable global healthcare providers to work as a team.” Plenty more examples to convince me never to write an article on geophysics, nuclear fission, or sewing.
















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…