News 6/9/15
Top News

Kareo is ranked by Black Book as the top vendor for integrated health records, PM, and physician billing solutions for the third consecutive year. ADP AdvancedMD, Athenahealth, Greenway Health, HealthFusion, McKesson, and NexTech also earned high marks.
Tweet Chat

Carly Medosch (@CarlyRM) will host the next #HIStalking tweet chat Thursday, June 11 at 1pm ET. Check out discussion topics here.
Acquisitions, Funding, Business, and Stock

The local business paper covers workplace clinic company Premise Health’s to evolve into a “patient engagement organization,” which will include a sharper focus on healthcare IT. Included in the Nashville, TN-based company’s plans are a patient portal, enterprise data warehouse, and customer visualization tools to help benchmark the company’s efforts.
Announcements and Implementations

Delaware’s Health Information Network selects IMAT Solutions to provide a secure system for aggregating, validating, and analyzing data from primary care providers and payers, then presenting the results in a scorecard user interface. The scorecard will be used by the HIE’s stakeholders to benchmark adherence to care standards, cost, and patient experience.

Orion Health integrates the eHealth Connect Image Exchange solution from eHealth Technologies into its Open Platform, enabling users to view, compare, and transfer medical images. The North Dakota Health Information Network will implement the combined technology its statewide HIE participants.
People

AMA President-Elect Steven Stack, MD is sworn in as the association’s 170th (and youngest) president.

The International Society of Telemedicine and eHealth elects Rifat Latifi, MD (International Virtual-e-Hospital Foundation and the University of Arizona) vice president.
Government and Politics
Representative Gary Palmer (R-AL) introduces HR 2652, titled Protecting Patients and Physicians Against Coding Act of 2015, which if passed would establish a two-year grace period during which both ICD-9 and ICD-10 codes would be accepted. It is the third bill introduced in the last two months that attempts to delay the upcoming ICD-10 switchover.
ONC seeks recommendations for procedures, tools, and test data to use in its EHR certification program. Among its needs: Identify the developer of test tools or procedures; specify the certification criteria it addresses; and explain how the test tool or procedure would evaluate an EHR or other health IT software.
Research and Innovation
An American Diabetes Association study finds that access to an EHR was integral to the success of certified diabetes educators in their efforts to help diabetes patients receive timely medication adjustments. CDEs often left recommended prescriptions for primary care physicians, who would act on them within a day. E-prescribing was presumably a vital part of that adjustment as well.
Weill Cornell Medical College researchers break down the Meaningful Use participation of New York physicians in 2011 and 2012. The study of 26,368 providers found that participation in the Medicaid incentive program rose from 6.1 percent to 8.5 percent, while Medicare participation rose from 8.1 to 23.9 percent. Not surprisingly, early and consistent participants had more financial resources and organizational capacity to support the use of healthcare IT, leading researchers to caution policy makers about the brewing of a digital divide and subsequent gaps in patient care in underserved areas.
Other

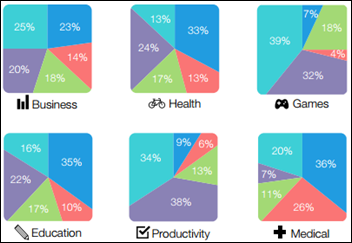
The AMA adopts a plethora of new policies at its annual meeting this week, including one that calls for the development of best practices to guide the development and use of mobile medical apps. Board Member Gerald E. Harmon, MD explains that, “This new policy builds upon existing efforts such as our partnership with healthcare technology incubator MATTER, our work with Healtheway and Carequality and our efforts to increase the appropriate use of telemedicine technologies.”
NPR highlights the hot market for personal, Web-based search information, calling out the CDC and WebMd for their hazy privacy policies and de-identified data practices. Data brokers are no longer using search information just to serve up a timely ad to the most appropriate user. The more nefarious often sell lists of users who have different diseases or symptoms to the highest bidder.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.





















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…