DOCtalk with Dr. Gregg 5/6/15
HIT Challenges of Being Independent (i.e., non-Borgian)
Being an independent physician these days sometimes feels like you’re a close relative of the Raphus cucullatus (dodo bird) – fewer and fewer of us to be found. Even with the increase in “concierge” or “direct patient care” practices, there’s a whole heap less of us unaffiliated, non-grouped-up guys and gals around.
Making decisions for a small practice is far simpler than those that large groups, institutions, and associations (the Borg) must make. Investigate, consider, decide, implement. No multiple meetings, no committees, no group think. Sure, you must be fully “fail fast” capable, but changing directions and making adjustments is so much easier and quicker when you’re small.
This is as true for deciding which office supplies you need as it is for which HIT you want to utilize. The only problem is that HIT requires a lot more thought, and yields much bigger disruptions if (or when) failure occurs.
Case in point:
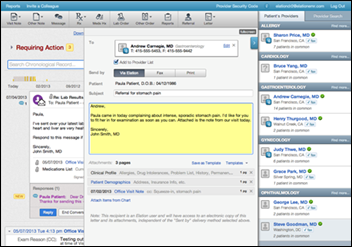
We have what I believe is perhaps the easiest to use EMR ever invented, Elation EMR. Maybe there are others coming along that will rival it, but I’d say our system can likely hold its own against any system for optimal user experience. Plus, it’s very cost efficient. It works just wonderfully for our little practice.
We also have an absolutely gorgeous patient portal, or “Online Care Center” as they call it, created by the good folks at konciergeMD. I’ve never seen its rival for functionality nor user experience, especially for pediatrics. Plus, it’s downright beautiful. Our patients/parents just love it and use it … and use it often.
I spent a long time looking for our first EHR (Bond Clinician) and enjoyed it. It had a rudimentary patient portal that we never implemented because it was clunky and ugly.
I spent even longer looking for our next EMR (Elation). We (my staff and I) have enjoyed it even more. It also has a patient portal, but it’s pretty vanilla. (Sorry, Elation folks; I love you, but your tremendous EMR experience isn’t matched by your portal experience.)
I spent longer still looking for a patient portal that I felt was easy, useful, and gorgeous enough to present to our families. The one we chose has our families actually using it, and feeding back very positive comments about it, on a regular basis. (Compare that to the oft bemoaned poor consumer adoption/use of so many patient portals.)

The rub is that choosing an HIT tool, regardless of the size of the company backing it or the company’s longevity to date, brings no guarantees. Our first EHR was from a startup (Bond) that eventually was gobbled up and moved up the food chain and corporate digestive tracts of MediNotes, then Eclipsys, and eventually Allscripts. Three of those companies, some older and much bigger than a startup, are no longer around. (And the fourth has had its issues.) And, of course, our EHR was eventually digested within the belly of Allscripts, excreted as now-forgotten digital stool, if you will.
The lesson? Big or small, there are no longevity guarantees regardless of which HIT product or vendor you choose.
Our current EMR is still thriving (I believe), but now our beauteous Online Care Center is about to go away. Well, sort of. The original company, konciergeMD, was acquired by Accolade. Accolade wanted the technology, but only wished to incorporate the tech into their tools. They sought to sell off the IP and rights to the Online Care Center itself, as they are not in the EHR nor patient portal vendor arena. Eventually, that is exactly what they did, though they sold it not to a company who would continue to offer it as an independent product. They sold it to an EHR vendor who plans to use it in conjunction with their EHR product. (I can’t blame them; it’s such a wonderful portal.)
However, this puts our little practice back into high tech quandary. Do we switch our patients over to the less-lovely and less-pediatric-friendly patient portal associated with our wonderful EMR? (A very cost effective move. Minimizes workflow disruption for us, though requires some change phenomenon for our families.) Or do we look for another patient portal to deploy? (Not many independent portals available. None as pediatric-friendly. Not nearly as cost-effective an option.) Or, possibly, do we consider switching from our wonderful EMR to this other EHR that now owns our favorite patient portal? (Tons and tons of ramifications there, the most significant of which is the workflow turmoil for our office wrought by such changes, something none of us enjoy.)
Such a dilemma.
I know the Borg face similar decisions, too. And their decisions often don’t have the fail fast capabilities that we enjoy. They often involve obscene amounts of money, too. Their HIT monies and the associated decisions are likely more than proportionally greater, too, as they often choose to go with very large systems from very large companies charging very large fees requiring very large implementation workloads and very large workflow disruptions. I sometimes feel a little sorry for them. (Consider all the reports you read these days of disgruntled providers – and patients! – who are stuck using various mega-systems that they find cumbersome, disruptive, and a plain old pain in the butt to use.)

I do so love being an independent. There are many, many advantages, and those advantages far outweigh the disadvantages in my book. While it might be nice to have others with whom to share big decisions, and maybe even share some of the blame when things don’t work out, I don’t think the tradeoff for innovative and adoptive adeptness is worth it. However, I must admit, when facing such situations, a little “Borgian-ness” might be more comfortable.
From the trenches…
(P.S. Would it be a first give up an EMR because of the patient portal, rather than giving up a patient portal because of a decision to switch EMRs?)
“Seven was a former Borg who had been human and had been assimilated. She was [now] regaining her humanity.” – Jeri Ryan
Dr. Gregg Alexander, a grunt in the trenches pediatrician at Madison Pediatrics, is Chief Medical Officer for Health Nuts Media, an HIT and marketing consultant, and sits on the board of directors of the Ohio Health Information Partnership.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.





















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…