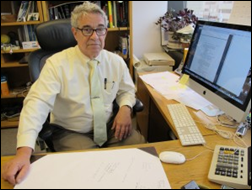
HIStalk Practice Interviews Baha Zeidan, CEO of Azalea Health
Baha Zeidan is co-founder and CEO of Azalea Health.

Describe how Azalea Health came to be, its current target market, and your role at the company.
Azalea was started by three founders, including myself, who worked at a regional medical laboratory company. In this role, I had the opportunity to work with many EHRs during the process of interfacing lab results and orders with physician EHRs. We noticed that most EHRs in the industry were clunky, and physicians had a hard time understanding how to use them because they did now follow their workflow.
In 2007, we recognized the opportunity to build a healthcare IT solution that would be truly cloud-based and as simple to use as an email tool. We offer a complete solution that integrates easily with existing systems.
Our target market has been focused on physician offices in small towns and rural areas. Our clients typically don’t have the resources or expertise to implement EHR and billing technologies that are now required by the Affordable Care Act. We help them with their workflow, revenue cycle, and compliance with government regulations like Meaningful Use and ICD-10.
I am the CEO and co-founder, and in this role I am responsible for driving the strategic direction of the company. With my team, I ensure Azalea Health is on track to meet its product development, customer service, and performance goals, as well as community goals. I have also, in many ways, become an ambassador for Azalea Health in our local community and in the healthcare IT community. Although I am the CEO and the visionary, every single person on the team has a say and contributes to our direction and success.
What is the status of the Azalea Health / simplifyMD partnership? Isn’t it really more of an acquisition on the part of Azalea Health?
Azalea Health has acquired and merged the simplifyMD team with our team. We are thrilled that simplifyMD customers are joining the Azalea family. simplifyMD customers will now benefit from an even greater variety of solutions and expanded capacity to support their needs. Azalea Health benefits from the addition of the highly talented simplifyMD team. It’s been a smooth transition and we are all excited about our future opportunities.
The current simplifyMD Atlanta office will continue to be in the Atlanta area. Azalea Health has its main office in Valdosta, Georgia, with satellite offices in Macon, Georgia and Gainesville, Florida. simplifyMD staff will not have to re-locate to Valdosta. We see the company as strengthening sales operations out of Atlanta with support and product development mostly in Valdosta.
One of the great benefits of this merger is how well the products complement each other. The product teams are working to interface products immediately and to determine the combined product road map.
Mike Brozino, simplifyMD’s former president and CEO, will continue to provide guidance and input in an advisory capacity. As the transition occurs, management team and roles will be determined and announced. We will continue to use Azalea Health and simplifyMD names and branding during the transition.
It seems that the EHR market, especially vendors that serve smaller practices, is living up to predictions of consolidation. What do you foresee your part of the market doing over the next three to five years? Are additional acquisitions in the company’s future?
You are absolutely right on your consolidation view. Actually, the recent transaction of Azalea and simplifyMD is a testament of that consolidation. The market is still highly fragmented, and companies with simple/scalable end-to-end solutions and with excellent customer service will continue to win.
I also foresee that physicians will start to work more with a vendor that can help them not only with the EHR software, but also with how to navigate the complexity of the financial side of our healthcare system.
We see ourselves as a leader in the industry, and we will continue to focus on growing our customer base organically and through mergers and acquisitions.
When do you think the replacement market will settle down? What do you think Azalea Health’s role will be once this happens?
Healthcare software is going through a major revolution, likely accelerated by healthcare reform. We see customers that are on a third replacement of their EHR. This trend will likely continue through the next decade as vendors attempt to keep up with the constant changes in ICD-10 and Meaningful Use.
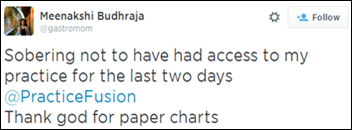
Some vendors have not prepared their solutions to keep up with rapidly evolving payment changes, and many will have difficulty in providing mobile applications for the providers and their patients. Also, as healthcare is becoming more and more interconnected, you will see some vendors not able keep up with the interoperability needed between systems – mobile, wearables, and clinical devices.
What are your customers’ biggest challenges at the moment with regards to healthcare technology?
Innovation and government regulation are causing healthcare technology to be in a constant state of flux. Navigating through the regulatory environment while simultaneously taking advantage of the most recent advancements from cutting-edge solutions is a daunting task for physicians and hospitals.
Providers are challenged by increasing costs, reduced reimbursements, escalation of regulatory oversight, and a need to ensure that their patient’s private health information remains private, all while providing the best quality of care possible. Our philosophy is to reduce the complexity of operating a medical practice by streamlining clinical and financial workflows, and providing services that assist with maintaining compliance and ensuring that the practice is adequately reimbursed for the services provided.
Have you seen any of your customers drop out of Meaningful Use, or avoid it altogether? Why have they done so, and has this been the best business decision in the long run?
We do see physicians dropping out of Meaningful Use, and we still see some that are avoiding it altogether. Some of them have avoided it because they see it as another layer of complexity in accommodating Stage 2, and they don’t see the advantage in doing more for less incentive.
Some are still on the fence thinking that they have a few more years to practice and maybe they’ll be able to dodge Meaningful Use altogether. This has not been a good decision for them for many reasons. More patients want to be engaged with their healthcare, and they are demanding that their clinical information be available electronically. Second, more providers are wanting to electronically send referrals and clinical data between health systems to different providers. Third, the healthcare payment system is going through changes (ICD-10, pay for performance, pay for outcome, pay for reporting). Those changes can be much easier to adopt if the provider is using a certified EHR and participating in Meaningful Use.
What are the company’s plans for next-generation product features? How will you ensure Azalea Health’s products stand out from the rest?
Azalea has a patent pending on “collaborative charting.” We are excited about this concept, which allows healthcare providers to collaborate in real time on a patient chart and see what each healthcare provider is documenting about the patient.
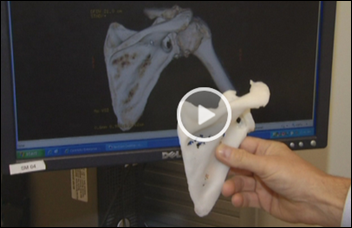
Also, we are very thrilled about our future mobile development. The next generation EHR is lightweight and mobile-focused. I can go on and on about our future development, including more tools for telemedicine – a key differentiator for us, as well as enabling device makers, patients, and other systems to easily and securely connect with the Azalea platform.
What is the company doing to foster innovation in your area of healthcare IT? Any future hackathons planned?
We had great success earlier this year with our first Azalea-sponsored hackathon in cooperation with local colleges and universities. We are making this an annual tradition. Also, we are planning this year on hosting an internal hackathon within the Azalea Research and Development Team!
Our VP of Technology, Duncan Kabinu, is starting a continuous learning and collaboration program within our R&D team that will look at potential innovations in new technologies, and not just those in healthcare. We’ll look to see how other industries have solved problems, and how we can learn from and apply those solutions in healthcare.
How do you see your customers responding to increased industry interest in telemedicine? Do you anticipate Azalea Health making a play in that area in the near future?
Telemedicine has been part of our strategy for several years. We have a project underway in which we are implementing the Azalea EHR in 40 schools in South Georgia in collaboration with the Georgia Partnership for Telehealth. This effort will help those schools use telemedicine in the school rather than taking the student patient out of school to see a provider or specialist.
We are also working on providing real time video chat within our platform to enable telemedicine and patient engagement. 2015 will be very exciting year for us, as we will continue to provide innovative tools for telemedicine and help connect rural patients with specialists from anywhere in the country.
It seems the company has a number of community service endeavors. Is there one service project in particular that has left a lasting impression?
Azalea Health has its roots in rural Georgia (Valdosta). We have been a huge supporter of United Way local projects. However, the most interesting and longest lasting projects we are involved in are related to helping our local schools, technical colleges, and state universities. We mentor interested students in programs designed to educate them about healthcare IT to help build and foster a local workforce that will fill our need for future innovators in the healthcare IT industry.
Any concluding thoughts?
The healthcare IT industry is going through a lot of change. It’s been very exciting to be able to help providers navigate those changes, and provide them with solutions that encourage them to focus more on patient care. Also, it is an honor for Azalea to be a company that helps patients learn more about their condition, while engaging them with their providers, and ultimately improving their overall healthcare.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.










































The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…