News 5/10/17
Top News

Boca Raton, FL-based Modernizing Medicine announces a $231 million investment from private equity firm Warburg Pincus. The specialty-specific EHR vendor has raised $322 million and acquired two companies – GMed and Aesyntix- since opening its doors in 2010. It anticipates using the latest round of funding to ramp up efforts around prior authorization automation, eCommerce platform development, data exchange and reconciliation, and telemedicine. Fred Hassan and Amr Kronfol, both of Warburg Pincus, will join the company’s board.
Webinars
None scheduled in the coming weeks. Previous webinars are on our YouTube channel. Contact Lorre for information on webinar services.
Announcements and Implementations

DocsInk adds CCM-friendly features to its charge capture services.
![]()
Integra Connect offers cloud-based RCM services for large urology and oncology practices looking to transition from fee-for-service to APMs.
TCI develops the SuperCoder Smart Assistant browser extension, giving coders the ability to look up codes without exiting whatever program they’re working in.

California Highlands and Recovery Centers of America (PA) select medication management and communications technology from Compliance Meds Technologies.
People

Michael Lovett (NextGen Healthcare) joins Formativ Health as chief commercial officer. It is the practice management services company’s third executive hire in the last two months.
Government and Politics

The Senate confirms Scott Gottlieb, MD as FDA commissioner. The cancer survivor was quick to respond to congratulations from NIH Director Francis Collins, tweeting that he’s looking forward to working with the NIH to “advance science in pursuit of medical progress and public health promotion.”
Research and Innovation
Findings from MGMA’s annual physician compensation and productivity survey highlight that pesky wage gap we’ve all heard so much about: Male PCPs earn 17-percent more than their female counterparts, while male specialists earn 37 percent more than women working in the same areas.
Other

The local paper covers OptumHealth’s impending acquisition of Reliant Medical Group, a Massachusetts-based group that has been independent since it opened for business in 1929. RMG CEO Tarek Elsawy attributes the decision – supported by the group’s 230 physicians – as a step in the right direction when it comes to remaining competitive. He explained that, “Reliant expects to bolster its ability to grow and expand, modernize many of its clinical facilities, have access to advanced data analytics capabilities, and attract top medical talent to its practices.”
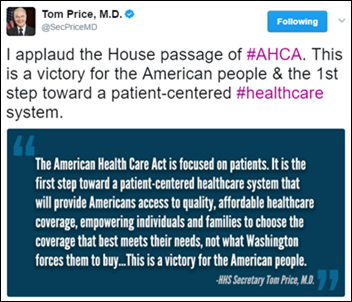
Authorities arrest Public New Service reporter Dan Heyman for “willful disruption of governmental processes” after repeatedly asking HHS Secretary Tom Price, MD about pre-existing conditions under the AHCA, and purportedly doing so in breach of Secret Service proximity protocols. The incident occurred during Price’s visit to the West Virginia State Capitol to learn more about the state’s opioid crisis.
Sponsor Updates
- NVoq will exhibit at the MGMA NE conference May 10-12 in North Falmouth, MA.
Blog Posts
- Consultants as Mentors? (Culbert Healthcare Solutions)
Contacts
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.































The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…