Steven Stack is president of the American Medical Association.

Congratulations on the AMA presidency! I know it’s been a year in the making. How will this coming year as president be different from the last year in terms of pushing forward AMA policy?
Thank you very much for that. I think it is a continuum. It’s the next step and next stop on the leadership journey of being able to contribute to what is really a team-based effort. The AMA has a long and rich history of working to help doctors help patients, and in the years that have led up to this for me, as part of the AMA board, I’ve had the opportunity to advance our efforts to improve health outcomes to accelerate change in medical education and to work to restore physician satisfaction and practice sustainability. As president this year, I have the privilege to be the individual on point, the primary spokesperson for that great work, whereas I was more part of the chorus in years prior. It does take a team. I look forward to continuing the work we’ve been doing for a number of years to try to make great progress in those areas.
What’s at the top of your to-do list heading into 2016?
I’m most excited about the things that we are doing over an extended period of time to try to improve health and wellness for patients and to support physicians in that work. Those are the three initiatives I just mentioned; the first being improving health outcomes, where the AMA is working very diligently to try to reduce the number of patients who transition from pre-diabetes to diabetes. We’re also working very hard to help physicians better identify and more reliably treat hypertension. Those two conditions alone are two of the most commonly encountered chronic health conditions in the American people, and the two of them combined contribute probably over a half trillion dollars a year to healthcare expenditures. We’ve partnered with YMCA of America, the Centers for Disease Control, Johns Hopkins University, and a number of other partners across those two initiatives in an attempt to reduce the number of people who become diabetic, and to better recognize and treat hypertension, efforts that we hope that will have a profound impact over an extended period of time on the health of the nation.
We’re also working to accelerate change in medical education. We are striving to boldly transform the medical school experience every bit as profoundly as was done over a century ago, such that the structure of the education and the content within the structure are profoundly changed to give physicians of today and tomorrow the knowledge, the tools, and the skills they need in order to succeed and provide the best possible care in the 21st century.
That leads to our final area, which is physician satisfaction and practice sustainability. The pace of change in healthcare – in the areas of technology and science, and payment and delivery structures – are changing at a pace that is daunting and that taxes any human being’s capacity to navigate it or keep up with it. A number of barriers have arisen in this process that keep doctors away from patient besides and mired in administrative work, clerical tasks, and non-value added steps. To that end, we’ve just released our Steps Forward modules, which you can find at StepsForward.org. Those modules are just the first 16 of what we hope will be more to come, where physicians use those if they’re applicable to their practice setting. By doing so, wee hope that they can shave hours of wasted time off their work week, time that will free them up to spend more at the bedside or to attend to their own health and wellness. At the end of the day, if we want a healthier, happier America, we’re going to need healthier, happier physicians caring for them.
I’m excited about those three areas particularly, but they’re all very big, very ambitious, and will take a lot of sustained effort. I would look at these at decade-long projects where we really hope to profoundly impact our profession and the patients that we serve.
What was the impetus for creating the Steps Forward program? How long has it been in the making?
It comes out of our commitment to helping doctors help patients. In 2013 we released our first of two Rand reports where we went out and tried to understand what makes doctors feel fulfilled in practice and what makes them frustrated or interferes with the work they do. We found that the single thing that made doctors most fulfilled was when, at the end of the day, they felt that they did good work. They’d helped patients be healthier and that they were supported in their work as opposed to interfered with. We also found the things that frustrated them. EHRs bubbling immediately to the top is the current most intense thing. There were other things like inefficiency, challenges with payers, complex systems that were difficult to navigate in a health delivery system. From that, we looked at multiple things: One, our advocacy; two, our partnership with other stakeholders; three, how can we create tools and resources for physicians to help them navigate some of that stuff and do better overall. The Steps Forward program is the outgrowth of that.
It currently has 16 modules. It’s open to all physicians. You don’t have to be an AMA member to access it. We are really committed to trying to help the entire profession to take steps within their personal control to feel empowered and to make their practice more fulfilling, more satisfying, and to navigate some of these complexities and the intrusions in a way that diminishes their negative impact. There’s modules about purchasing an EHR or deploying it. There are modules about how do to preplan a patient visit to the office differently so that some work is done before arrival, which then allows the doctor and patient to make better use of their time at that initial visit.
We also have an opportunity for physicians with good ideas to submit them online for judging by an outside panel. For those physicians whose ideas are selected, we’ll provide a $10,000 award in return for their partnership in helping to take their idea and develop it into new modules for the program. That can currently be seen on the Steps Forward site, and I’d certainly love it if you’d share that in this column, because we want as many physicians with good ideas to come forward so that we can create bigger and better tools for more physicians. We are committed to preserving a robust platform and program to benefit the entire profession, and are pretty excited about that.
How will your experience as an emergency physician inform your work as president?
I think all of us who are physicians are strongly influenced by the specialty that we practice. And in my particularly specialty, I think the emergency department is a really profound, oftentimes saddening lens on society, where we see many people working very hard to do good things and help patients, but in a system that is complex, inefficient and challenging to navigate. We also see where patients who have really significant needs are unable to have those needs met because society does not have in place the resources and the support structures needed to care for them.
I told some stories in my inauguration address, all of which are from my own personal background of practicing emergency medicine, where people turn to the ED because they have no other place to seek care. They turn there because they’re lonely and they seek comfort or compassion or social engagement. People who have become addicted to opioid medications, who struggle with a life of misery and terror, trying to grapple with that and finding scant opportunity to get help and to get better. Having that perspective will help me, I hope, communicate the need to work very hard to make things better, to collectively try to improve the system. At the end of the day, we are all committed to the same purpose. We want to make sure that people have the healthiest, happiest lives they can, and that society and the people in it are as productive and contributory to it as possible. I think my particular specialty background is just an uncommonly broad lens into society across all levels of education, all levels of wealth or poverty, all levels of urban or rural or suburban settings.
What were the hot healthcare technology topics at this year’s AMA meeting?
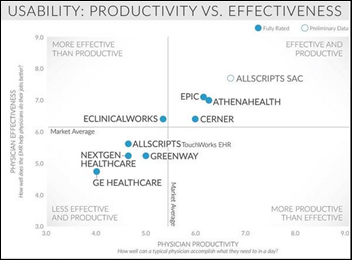
Two topics rise immediately to the top, and then a third that’s fast coming down the road. The two that rise to the top are EHRs and ICD-10. The one fast coming upon us is mobile – both apps and devices. As far as EHRs go, we have really good data. We know from a study we did with Rand in 2013 that more than 80 percent of physicians have no desire to go back to paper and pen. They want to use EHRs. That being said, it is nearly universal that physicians have great frustration with their EHRs. The current generation of tools all too often interferes with patient care. They certainly degrade our efficiency. They certainly take us away from talking with patients because we’re endlessly clicking a mouse or typing into a software program that’s cumbersome and clunky. It’s more like using an old Apple 2E when we had the blinking C prompt in BASIC than it is anything like an Apple iOS operating system on a mobile device.
Physicians are very frustrated with these systems, and then we’re very frustrated that the Meaningful Use program that we’re all subject to is overly prescriptive. It lacks flexibility where needed and has compelled us to purchase non-functioning tools to use them in ways that degrade our practice. Let’s not forget that more than half of Medicare physicians are being penalized by Medicare with a one-percent reduction in compensation, because the tools that we are given are so poor and the program the government created so rigid. Now we’re being punished for our inability to achieve what I think, if we really discuss it very openly, is a program that isn’t well-designed and sets us up for failure. Needless to say, EHRs continue to be a challenge, and physicians are very frustrated that their input has been disregarded in ways that are injurious to the work we’re trying to do.
As far as ICD-10, AMA continues to believe that the costs incurred and the potential negative consequences we may experience do not justify this transition. We certainly recognize that so many others in the healthcare enterprise feel differently, and are at this point fairly insistent that it will happen and we’re going to go forward with it. If it does go live on October 1st as is currently scheduled, we really strongly believe there’s a need for a grace period where physicians are not punished simply for failure to have a sufficiently specified code. We have advocated and continue to advocate that CMS make use of its prepayment authority to ensure that claims get paid in a timely manner, and that physicians not be denied payment simply for a lack of whatever is the newly perceived level of specificity that’s desired. And that CMS also commit to not subject physicians to future fraud accusations simply for the learning stages of the new code set. We’ll continue to work with CMS on those points. I think everybody wants to have a smooth transition. I don’t think anybody is advocating for chaos or anything less than a smooth transition. We just continue to feel not enough attention has been given to the contingency planning and the advance planning.
The third and the final thing is mobile. Everybody has a smartphone these days, and mobile is prevalent. More and more Americans are turning to their mobile devices and apps to try to help participate in their healthcare, so this is an industry that is already large, growing rapidly, and has great promise when used appropriately to empower patients to better manage their own care and health data. But if done poorly, it could also challenge or threaten the security of patient’s private information. It could also perhaps cause harm if misapplied. We’re excited about the positive possibilities here, and I think appropriately cautious about the need to attend to the details so that the negatives don’t get in the way of the positive progress. We look forward to continuing to work on the evolution of mobile devices and apps and what their role is appropriately in the medical enterprise.
I want to play devil’s advocate and ask how you’ve seen healthcare IT help put joy back into a doctor’s daily routine?
As an emergency physician, I work in a fast-paced, information-poor environment. Health IT enables me to quickly look and see a patient’s prior EKG, laboratory, and imaging data. That’s great information. It helps me provide better care for patients. Being able to communicate with the pharmacy using electronic prescribing is also a wonderful thing. So I think that there are instances where health IT has been very helpful. It’s just that the interfaces are very clunky, and we are compelled to put way too much information in structured format, which requires clicking and double clicking and triple clicking on a mouse to select all sorts of things in a structured manner. That’s inefficient and really tedious. The notes themselves lose the storytelling aspect of healthcare, where we can actually make your specific scenario come alive with what is unique to you and your health needs and concerns, as opposed to everybody who has a chest pain looking exactly the same because the EHR spits them all out looking identical. I would say there’s a need to work through those challenges. Health IT has been helpful and will be far more helpful when these records are actually interoperable. We’ve created digital silos that don’t share information any better than the old system where we had to have people send information via fax machine. If the federal government and software vendors would work much more attentively on making these things interoperable for those things that are of high use to us, I think that physicians would find a lot more joy from the tool than just the current reality where they contribute more misery than joy.
Do you have any final thoughts you’d like to share?
It is an incredible privilege to be a physician. And I think patients should know and take comfort that physicians are at our best, are most fulfilled, when we really feel we’re doing good work to help them meet their health and life needs. I know that there are a lot of complexities we have to navigate. The AMA, and I as its president, are committed to trying to navigate those complexities, to have barriers and impediments not get in the way of doctors and patients working together as a team to advance their health and wellness. I think it is an incredible honor, in addition to being a practicing physician, to now also have the opportunity to convey the really good work the AMA is doing in things as big as health outcomes, medical education, and physician satisfaction. I think that it’s a great privilege. I feel very fortunate to have the opportunity, and I look forward to a great year ahead of good work for patients and the physicians who serve them.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg, Lt. Dan
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.



























Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…