John Meigs, MD is president of AAFP and a practicing family medicine physician at Bibb Medical Associates (AL).

Tell me about yourself and the organization.
As you probably know, the American Academy of Family Physicians is the only medical association completely dedicated to primary care. We’ve been around since 1947, so we’ll have a 70th birthday next year. Now, I have not been a family physician for quite 70 years, but I have been a family physician since 1979. I actually practice where I grew up, in Centreville, AL – about half a mile from where I graduated high school. The greater metropolitan area is about 5,000 people. I was in private practice for 31 years, and then in January of 2013 merged with another physician to move across the street. I’m still seeing my same patients and pretty much in the same location, but the address changed from 223 to 208 Pearson Avenue.
Now that you’re president of the AAFP, do you still see patients on a daily basis?
Though I travel a good bit for my academy job, I’m still what I call a real doctor. I still see patients every day – about two dozen in fact.
The release of the final MACRA rule is still making headlines. How do you and the academy plan to help family physicians transition to its value-based programs?
We have been working actively to educate our members about MACRA, letting them know that they need to participate as soon as they can, as fully as they can. This was a long, complicated rule. We’re still studying it, and as we delve into the rule, we will continue to educate them. We’ve got a designated website for our members. We’ve already put out a readiness assessment checklist. We’ve got an FAQ … there’ll be more information to come. [The AAFP released an executive summary of the rule earlier this week.] We’re trying to make our members aware, and then let them know the details as we are able to parcel those out and advise them on what they need to do.
We have long asked and thought that primary care needed to be paid differently; the old volume-based system for our specialty was just not in our best interest, and we’re hoping with a transition to value-based payment that it will be once our members get through the transition and get their ducks in a row. I’m hoping it’s going to be a positive experience for our members.
Do you think family physicians will welcome this transition, or is it seen as another regulatory hurdle they have to get through? What are your thoughts based on what you’re hearing from colleagues?
Well, change is frightening. Initially there’s going to be … I don’t know if fear is the right word, but there will be the trepidation of change and doing something different. Fear and anger trump truth and fact all the time, so until they get to know its ins and outs, there’s always going to be that fear and apprehension. As I said, as they become more familiar with it and are able to participate in the value-based system and the quality payment program, we should be all right.
That being said, this has not been front and center for the majority of physicians, family medicine included – the folks that are just going to work everyday seeing patients. It’s similar to when ICD-10 came out a year ago. For awhile, folks just sort of ignored it until it was upon them. Well, MACRA is now upon us, so I think that will begin to get their attention. We’re doing everything we can to increase its visibility and emphasize its importance.
How do you think healthcare technology is going to help – or hinder – physicians as they move to value-based programs?
Let me be circumspect about what I say on this one … Health IT is foundational to the transition to this new payment system, but right now, it’s more of a hindrance than a help. We’ve got to get to the point where the IT aids us in the care of our patients and the care of patient populations instead of being a roadblock to care. It’s got to get to the point where it’s a natural part of the physician’s workflow, where the computer does not come between the physician and his patient. It’s got to be interoperable. You’ve got to be able to have access to information without the problems we have now. We’ve got to get away from checkbox medicine. We’ve got to get to the point where we’re using this IT for the benefit of our patients, not just for the benefit of the bean counters. Right now, there’s too much administrative complexity. The complexity of modern medical practice is now the number-one cause of physician burnout.
Why did you decide to leave independent practice to become affiliated with the hospital that you’re now practicing at? Did health IT and/or administrative expenses play a part in that decision?
Now, I want to be clear – I am an advocate of health IT. I have had a computerized system in my office for 20 years. I’m on my fifth system now. I don’t want to repeat everything I said awhile ago, but the current IT systems are literally designed to maximize billing. They’re designed for bean counters. They are not designed for patient care. That’s the problem. As I said, I’m on my fifth system. I hate them all. There’s not one out there that does what it ought to do despite what they claim.
The other problem I have is they set up this certified health information technology program. When you get a certified system, you assume when you’ve spent that money that it’s going to do what it needs to do without you having to buy additional modules. We’re making these IT companies rich, and the government’s not holding them accountable. Their interoperability standards that are in the law … we’ve got to comply with the law starting in 2017 and they don’t have to comply with some of these until 2025. That’s not right. The vendors need more skin in the game. They need to be held accountable.
Let me get off my soap box. Sorry about that. I don’t think I even answered your question. When I was in private solo practice, I had a real desire to be more involved with the AAFP. I knew I wanted to run for president, and I had been on the board for a few years. I was working 40 weeks a year with 52 weeks of overhead. One reason was financial, like I just mentioned, and the other was my AAFP travel schedule. I wanted to have a way for my patients to be taken care of while I was on the road. I had the opportunity to merge with another physician, and the hospital was interested in building a clinic. We merged our two practices into the new clinic there. It’s actually located inside the hospital, but it is a physician’s office. We’re just two halls over from the emergency room. It’s convenient, and we’ve got easy access to the hospital.
Aside from MACRA, what are your priorities for the academy and its members during your term as president?
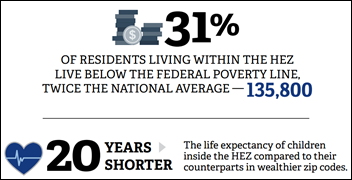
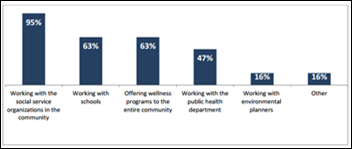
Other than MACRA, the big national issue that’s getting a lot of press and publicity is the opioid epidemic, so helping to address that is something that we will focus on. The other issue has to do with workforce. We need funding reform that’s based on the actual physician workforce needs of this country. Another issue that I think is very important is diversity and working on the social determinants of health. We know as family physicians that it is critical to meeting the healthcare needs of our patients and our populations. When folks don’t have a safe place to sleep or access to good nutrition, sometimes writing a prescription is not the most important need that we should work on. And of course we need to reduce the administrative complexity of modern medical practice.
Does anything about healthcare IT excite you?
The potential. Health IT has tremendous potential. Current systems have not reached their potential. When we have access to data in a meaningful, real-time way where we can make decisions that not only affect the health of our patients but of the populations that we treat, it’s exciting to think about not operating in a silo, but operating where you can make decisions based on large aggregate data and do what’s best for a patient.
The other thing with IT is that you can do more things remotely. We can take care of folks and it doesn’t have to be just in a face-to-face office visit. That’s why I think over 10 years from now, healthcare will be radically different from what it is now. I may be taking care of you through a portal and through smartphones and other things, and you may actually only come see me every year or two if something pops up that we can’t handle, or just to make sure things haven’t changed. The problem with our current system is that we’ve got to be able to survive in our practice through this transitional period until we get to the point that we reach this potential. There’s tremendous potential, but not with our current system.
Do you have any final thoughts?
We must reduce administrative complexity! But seriously … I can’t think of anything else I need to add.
Contacts
Jenn, Mr. H, Lorre, Dr. Jayne, Dr. Gregg
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.

























Re: Walmart Health: Just had a great dental visit this morning, which was preceded by helpful reminders from Epic, and…