HIStalk Practice Interviews Caraline Coats, Vice President, Provider Engagement, Humana
Caraline Coats is vice president of provider engagement at Humana.

Tell me about yourself and the company.
I am the vice president of Humana’s Development Center of Excellence department. We are largely a team that supports Humana’s enterprise goals around our value-based journey, supporting our physicians and their overall experience as they move from volume to value. My team supports our network and our market leaders on choosing the right physicians – those who make good partners. We want to develop a long-term understanding of what their needs and capabilities are and meet them along the way on our continuum. Humana doesn’t really have a one-size-fits-all. We have different options to meet physician needs depending on their infrastructure, capabilities, and appetite to launch from volume to value. My team serves as the internal operations support for our value-based goals.
My background is historically more of what you call your traditional managed-care contracting and more transactional oriented. I’ve worked both with physicians and in the hospital space in doing contracting and negotiations, and have also served in leadership roles with Humana in our network organization. It’s been within the last four to five years that I’ve transitioned myself from what I’d call the volume to the value world. I feel like I’ve been making that journey in parallel with our physician community. As the industry is evolving that way, Humana is growing its own capability to support physicians in that space.
When did Humana launch its provider quality rewards program? How have you seen provider interest in that grow?
Humana has actually been in the value-based space for over 20 years. We have had what I call a more standard physician rewards program for the last five or six years, and it’s really progressed as the industry has progressed. Outside of the markets that have been more mature in it, the program is offered to engage and support physicians early on around certain quality metrics. It provides financial and clinical data to manage that core, founding population. We work with them along the journey to determine if and when they’re ready to move beyond just upside only and take some element of risk.
We start with physicians early on, looking at opportunities and ensuring that they’re provided with adequate data that is actionable around their population. We help them grow critical mass with them, mitigating any volatility in the numbers to help move them farther along that continuum where, eventually, they can share in some of the upside and downside risk.
How does Humana recruit physicians for the program?
We don’t have a formal recruiting program. We have a lot of local resources on the ground through our market and our leadership team through building relationships with physicians and understanding what their needs are – what programs we can offer to meet them along the way. We have over 900 value-based relationships and that continues to grow. We have increasing goals each year to put more and more physicians in our value-based programs, but I emphasize it’s not just around the number. It’s around really finding the right partnership and the right place on the continuum. I think with that it’s not so much a recruitment as it is just building deeper relationships with our physicians and finding out how we can support them.
How has technology impacted the ability of practices to succeed in your value-based programs?
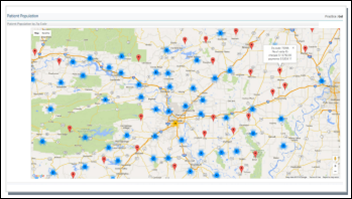
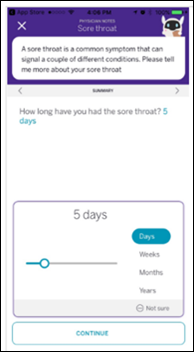
Technology is critical to a physician’s ability to effectively manage population in the value-based space. Humana does provide some population health capabilities that provide financial and clinical data to the physicians around the population that they’re managing. We now have an increasing utilization of this capability from the physician’s self-service perspective. Historically, we have provided the data and the reports directly to them, which we continue to do but are now allowing functionality where they can access it themselves and use that data to turn it into actionable information to manage their population.
How does the quality rewards program fit into physician plans to participate in MACRA and its quality-improvement programs?
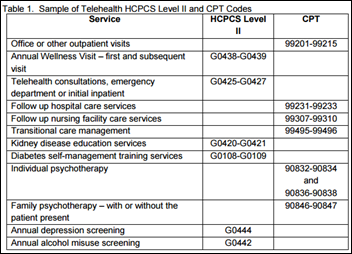
We’re all learning about MACRA. At a high level, it’s value-based, so MACRA is CMS’ way of moving physicians from just volume to value, and rewarding them for improvement in quality around certain metrics. I would say the fundamental feature of our value-based program does that. It has quality metrics built in and we work with the physicians on measuring, improving on, and rewarding for those metrics. Fundamentally, the concept is the same. How our program evolves to align with MACRA is in progress. We’re determining what will make the most sense for physicians to mitigate a lot of disruption, but continue an improved experience where ultimately their patients are getting the most high-quality care.
Aside from the quality rewards program, how is Humana helping physician practices implement population health management programs? You alluded to data earlier. Are there any other ways you’d like to highlight?
Yes, continuing evolution of the data and actionable information that we can provide to them. I don’t want to underestimate the local resources that we have on the ground. We have regular joint operating committees with our value-based physicians to review data, understand obstacles and barriers, and understand what they need to continue successful evolution in their value-based programs. That face to face relationship with the physician I think is instrumental to continuing success.
Outside of that local market level, we now have value-based executive care forums that are led by our office of the CMO. We call in value-based physicians from around the country and have a day-and-a-half session – an open forum – so they can learn from each other, we can hear directly from them and understand how we can support them in population health.
Given the direct feedback you’ve received, what are the biggest barriers practices face when it comes to implementing population health management or value-based programs, and how is Humana working to help practices overcome those barriers?
One of the biggest things we hear, and it’s not unique to Humana, is that we need to do something different for everyone. Even looking at MACRA coming up, what does that mean? To report different data when you have traditional Medicare, plus a handful of health plans … it’s the different offices and the different programs. Payers including Humana can look at how we can provide a physical solution to them to improve the administrative burden, if you will, of all those different programs so that they can focus on patient care and adhering to one program that ultimately meets the quality of their patients and improves their experience.
Do you have any final thoughts?
No, other than Humana recognizes the world of value-based care is evolving and every physician’s need is different, every practice’s need is unique. We continue to learn from each market and each physician, and strive to evolve our programs, options, and capabilities to best meet them where they are so they can successfully grow in this space.
Contacts
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.


























The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…