HIStalk Practice Interviews Mark Tomasulo, DO Founder and CMO, PeakMed Direct Primary Care
Mark Tomasulo, DO is founder and CMO of PeakMed Direct Primary Care in Colorado.

Tell me about yourself and the organization.
I started medical school a little later in life. I started undergrad at about 25 or 26 years old. I spent four years in the Navy. I was an airplane mechanic, and then worked as a civilian for the government, and ended up hurting myself, and used the GI Bill to put me through the first two years of undergrad school. I got a scholarship for the second two years of undergrad, and then when I got accepted to medical school, I applied back to the Navy, as well as the Army. I liked the Army package a little bit better, and so they helped put me through medical school. In doing so, I spent about eight years in the Army, and four years in the Navy prior to that. All of my time in the Army was spent as a physician. I did my residence training at Fort Benning, at Martin Army Community Hospital. Then I was attached to the Big Red One, the 1st Infantry Division. And then got stationed at Fort Carson after a deployment to Iraq.
When the time finally came for me to decide whether or not to stay in the military, I ended up going into the civilian workforce. I spent a lot of time in the ER as an ER physician, as well as an urgent care physician. I really started to understand the barriers to healthcare when it came to civilian medicine. I’m a family physician, board certified, so my heart has always been with primary care, and so working in the ERs and the urgent care facilities, I really started recognizing that most of what we deliver in the ER is primary care. It’s lack of access to your primary care physician that forces you into an environment like the ER. I would venture to say that 95 percent of all urgent care visits are truly primary care visits. There’s a lack of access to primary care that has allowed urgent care facilities to flourish throughout the country over the last 10 years.
Lack of primary care access and the cost of living in a high deductible health plan world has created an environment where the patient waits until the very last minute to go see a provider. We’re living in a sick world, not a healthy world. And that’s why PeakMed was founded. When I started the company, it was really to solve the equation of access to your doctor, and the cost of going to see your primary care physician – to change the economic model, creating a viable primary care practice outside of third-party payers.
What role does technology play in PeakMed operations?
I think technology in the 21st century is a massive resource and a powerful tool, especially when you put it in a healthcare space. PeakMed really looks at technology as a means to providing care to our members in a manner that suits them best. Whether that care is through a brick and mortar location, like a traditional setting, or a text message, an email, or even telemedicine. What we want to do is leverage technology so that it enables access for our patients, creating an exchange of information between a doctor and a patient, so that the patient feels like they are taken care of, when it’s convenient for them. When all of those things work out well, and you allow your physician to drive that relationship, technology is a really key component to care access.
We use a lot of technology on the back side of the practice, which allows us to validate what we’re doing for our patients. It allows us to validate our model, compared to a fee-for-service environment, to see if we’re actually taking better care of our patients. It creates a way for us to validate what we do, and how we do it.
Do you use a traditional EHR and PM system?
It’s a combination of a lot of things, because what we do is outside the norm of a fee-for-service clinic. A typical EHR is really based on transactions. It’s based on the ability to code for a specific encounter that allows the practice to bill for that event. It also, as a system, provides a technology that allows you to measure population health inside of your practice. It prompts providers to do specific things for a specific type of patient. With our EHR, we don’t concern ourselves with having to code an encounter for the purpose of reimbursement. We want to be able to quantify that encounter, or the visit, for population health measures and for internal purposes that allow us to improve our delivery model.
We do use an EHR, but we also have created our own technology because there was none available that allowed us to start looking at claims data for the total cost of care on a patient by patient basis. It allows us to really start identifying where the patient is spending money in the system, where we can influence some of that spend outside of the scope of primary care. It helps us understand where the money is being spent, and how much we can impact that outside the scope of primary care services in a way that helps us validate the savings that we generate for our members, as well as our employers.
You’ve mentioned that PeakMed will start looking at telemedicine, courtesy of a recent $5.5 million funding round. Why now? Are you looking at certain vendors?
We have lots of strategic partners in terms of technology platforms. When we talk about telemedicine, it’s a functionality inside of our encounters, or our EHR, that allows us the ability to have a video conference with a patient. Do we use a vendor like TelaDoc? No. It’s a totally different model. We use technology to make the connection face-to-face, through video. Everybody knows that as telemedicine. We don’t need a vendor in order to do that, but we do have some strategic partners that provide the HIPAA-compliant environment in which that occurs.
Is PeakMed looking at adding mental health or behavioral healthcare services?
Yes, absolutely. In our country, it’s one of the more underserved areas of healthcare. We need to start changing the way we talk about behavioral health and the way patients access it. And, once again, the cost that’s associated with therapy. To answer your question, the answer is absolutely. We have created a partnership with a behavioral health organization that is going to deliver behavioral healthcare to all of our patients, in our clinics, under the same type of membership model. You’ll have one fixed cost that includes PeakMed and behavioral health, which is done inside of the clinic. Everything from pediatric psychology to pediatric psychiatry, adult psychology, adult psychiatry, addiction counseling, group counseling, individual counseling. Those will all be offerings inside of our per member, per month cost.
Circling back to technology, how have you seen it improve access and outcomes at PeakMed?
Patient buy-in to management of their disease is critical to increasing compliance, which influences outcomes. If I can diagnose a patient with diabetes, have enough time to explain what diabetes is, more time to explain how we’re going to manage it, and then allow the patient to ask every question they can think of .… If those things can happen, and I have buy-in from that patient, the compliance is enormous. And the return on compliance influences the outcome of that disease. It’s all about exchanging information and knowledge. If we can use technology to help facilitate exchange of information between a doctor and a patient, it allows us to really start changing how we manage, and how we influence, a disease state.
For example, in the fee-for-service environment, patients are typically seen by the physician 1.4 times per year. That’s a national average. Inside of our facilities, we’re at about six times per patient, per year. We engage with them more frequently than the traditional model of care because we have time for the providers to reach out and be proactive and preventative with our patients. In doing so, the compliance, the outcome, the quality, the satisfaction, and the reduction of total cost of care is enormous. If I can keep the diabetic patient from an ER visit and an ICU admission, which can potentially cost $100,000, that’s an enormous win for PeakMed, the patient, and the healthcare industry. We’re saving money from every angle that we can think of, and we’re using technology to help facilitate that.
Healthcare in this country has been under enormous strain over the last several years, in terms of policy, cost, and access. Have you seen this drive interest in the direct primary care model?
Yes, I believe it has, but I think what it’s really done is creat an understanding that there’s a massive difference between healthcare, and health insurance. I think the ACA was always about health insurance reform. It wasn’t really about healthcare reform. With health insurance reform, it’s created an environment that is exceptionally expensive for individuals. They feel like they’re paying more on an annual basis, and getting less every year.
We need to shift the conversation to help consumers understand the difference between health insurance, which is really there to keep you out of medical bankruptcy, and healthcare, which is there to prevent you from having your hypertension lead to a heart attack or a stroke. People need to understand where their money is going and what value they’re getting. Today’s health insurance environment has led individuals to look for solutions outside of a traditional model. There used to be a time, 20 years ago, when health insurance was very synonymous with healthcare. I think those times have changed dramatically, and I think PeakMed is really starting to impact the healthcare component, and helping consumers and employers understand how to purchase both those things in a transparent, conscientious way.
You mentioned in an interview several years ago that the biggest challenge to being a physician was politicians, government, and bureaucracy. Do you still find that to be the case?
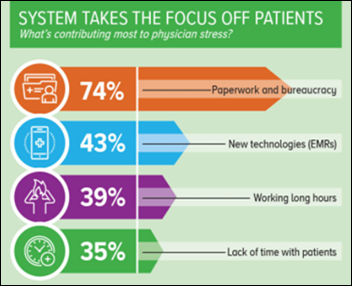
I think when a practice is required by a government entity to validate what they’re doing, in the form of creating more administrative burden … I think it’s very discouraging for the practitioner to continue doing what they’re doing. What a doctor really wants to do is take care of a patient. The more administrative burden that you place upon a doctor takes away from the patient/doctor relationship. It leads to a tremendous amount of burnout in our industry. I think a lot of physician burnout stems from the administrative burden that it takes to maintain a viable practice.
I think there are a lot of similarities from several years ago that really haven’t been fixed. They may have even gotten worse. Reimbursement-related mandates, for example, put a lot of pressure on the practice, and I think it creates a wedge between a viable practice and patient care. The doctor has to make a choice at some point. I think those are still very valid barriers in our current system that haven’t been addressed through legislation, or politicians. It’s going to take some innovative companies like PeakMed to create a solution and share it with others – a solution that shows a different way of practicing medicine, and an economic model that allows it to be viable.
Contacts
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.



















The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…