Justin Barnes is chief growth officer at IHealth.

You left Greenway in early 2014 and recently joined IHealth as a partner and chief growth officer. How did you fill the time in between?
My number-one priority when choosing to depart Greenway, which was a very difficult decision, was to take a little bit of time off to just recharge the batteries. I had my hands in three fairly large pots in the industry. Greenway was one of them. I was doing a lot of work on Capitol Hill and then also helping to start and lead several industry associations. I was running in a lot of directions for well over a decade, and it was time to pull back a little bit, to reflect on what I’d been able to accomplish, what I still wanted to do, and where my passions were. To figure out what’s next, I believe you’ve got to slow down, reflect, and really be deliberate about your path of life. For you, for me, and for a lot of our friends, our work is intricately involved with our life in general. We compartmentalize probably fairly well, but we’re very passionate people, we all care about healthcare, our society, and our country, and so you just can’t separate them morning, noon, and night. It’s all interwoven.
I know you have a real soft spot for entrepreneurs. How did you stay in that world during your downtime?
I’m very faith-based, as you know, and so I prayed about it. I didn’t want to take myself too far out of entrepreneurialism and fortunately was introduced to ATDC, the Atlanta-based Advanced Technology Development Center, which is a technology incubator out of Georgia Tech. It was kind of love at first sight in a way. They saw my background and wanted to get me more involved with the 12 companies they had at the time. That was a great opportunity to see what’s evolving in the industry and how startups are managing today. It was really interesting to see how running a startup is different than it was when we built Relay Health and then Greenway. It’s very different today.
What drew you to IHealth?
I’ve always felt that navigating care providers is the future of healthcare. It’s what I did with Greenway. It’s why I did all the public policy work. It’s why I did all the industry association work. With Greenway, and a lot of the industry, it was all about innovation technology; that’s kind of where the industry was at the time. Now, with all these evolving payment and care delivery models, it’s about service. It still comes down to hands-on service – helping providers, sitting with them, and navigating them through their challenges, which are increasingly related to moving them from fee-for-service into value-based care.
During my time off, I asked myself, how do I continue on this mission? This is still my mission. It really and truly is. Again, it comes back to faith. I prayed about it and then happened to run into a good friend of mine who is a partner at Fulcrum Equity Partners, a private equity group here in Atlanta. He’d loved what I’d done at Relay and Greenway, and wanted to try and find a way for me to work with Fulcrum. They introduced me to a company that was looking to do a couple of acquisitions. When I met with them, they were all about revenue cycle and they’ve done very, very well on that side of things.
Another company that they were looking at acquiring did very well, again, on the revenue cycle side, but also had a great customer base in the hospital environment. One side of the business that was growing, IHealth Solutions, was really practice-based, focusing on credentialing and revenue cycle. The other company they were looking at, called DNA Health, was looking at the hospital market, but did some practices as well. They focused on revenue cycle, but also had care coordination, population health, and analytics. When you put those two organizations together, you have the full suite of innovation-enabled services for the practice market as well as the hospital market. That’s when I said, wait a second. That is the secret sauce to helping providers navigate the future of healthcare.
They were leaning on my knowledge and expertise to really fashion this type of opportunity into something more substantial, and so that’s really how it all came together. It was meant to be. It was just three business partners that we congealed very quickly, very well. These were very mature organizations in their own regard, but coming together made them much stronger. I think today they have over 300 employees globally. We’re off to the races.
How is IHealth poised to help physicians move to these new value-based care models. What does that actually look like to your average MD working daily in the trenches?
I see it as two parts, maybe even three. The first part is, let’s look at what you’re doing today. Every single practice, and hospital for that matter, that we walk into has so many inefficiencies and opportunities for revenue. Despite what they’re already doing, they’re not getting paid anywhere near what they should be. You and I, we would never stand for that. If I work, I should get paid fairly and compensated for my work. Most providers feel that way, but they don’t have the innovation or the service to be able to capitalize on that and optimize that, and so the number-one step is to stabilize where they are today. Optimize their fee-for-service contracts, make sure they’re getting paid properly based on their fee schedules, make sure their denials are as low as they possibly can be, send out the cleanest claim, authorize 100 percent of patients before you put them through the entire process, and make sure all the doctors are credentialed.
I can’t even begin to tell you the tens of thousands of dollars going to practices and millions of dollars that we’re requesting for hospitals on top of where they were. We’re unique in that we go 100-percent at-risk. We don’t charge a nickel until we collect additional revenue for you. We’ll stabilize where they are, optimize where they are, and even help them modify some of their EHR templates and reporting to get additional money. We also look for risk-based contracts they might be able to engage in. IHealth has a whole team dedicated just to that. Then we’ll go back and educate the practice on what they can do. Once we register them for qualifying programs, then we’ll modify and customize their EHR for capturing all those metrics and then manage that to make sure they’re hitting red light, green light, yellow light ….
We’ll manage it all through our dashboard and then produce your analytics, your reports, and then attest for you. It really is soup to nuts. No one has ever done this before in the history of healthcare that I am aware of, going in 100 percent at risk. It’s all service. This is really going from stabilizing to optimizing to properly positioning them for tomorrow.
You mentioned that the world of startups is different than it used to be. How has the revenue cycle world changed over the last several years? What sort of challenges are physicians faced with now that they may not have faced five years ago?
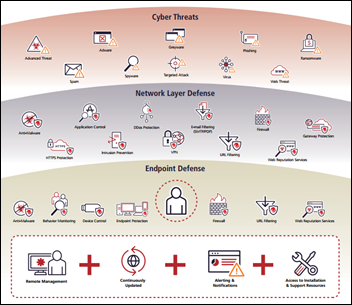
The revenue cycle world is completely different than it was even three years ago. Payment models are becoming much more complicated, not just with ICD-10 but with fee schedules and risk-based contracts. Hospitals and practices are under more pressure and they are having their payments held up more than ever before by payers and others. This is very complicated and I’ve got to be very respectful here. The doctors need an ally on their side. I know how to go get that money, how to manage their revenue cycle so that they can go collect a fair amount of money from their payers. Right now, money is being held up through no fault of their own. It’s because there are many more complexities and a lot of the billing staff just don’t have that expertise to file that claim cleanly initially with all the right authorizations so they can get paid much faster.
This has changed so dramatically over the last probably two years. You now have to have a completely different RCM strategy if you want to get paid. Most providers have got to be off by 15 to 20 percent, if not more, if they haven’t changed anything in the last couple of years, and I know that from sitting with them. That’s just traditional fee-for-service, never mind once you layer on a risk-based contract or any type of value-based care contract. That’s another conversation altogether. We call that revenue cycle performance, which is allowing you to get paid for what you’re doing and optimizing what you’re doing.
It seems providers are getting hit with something every few months, whether it’s a new federal program or deadline of some sort. Have you ever seen this pace of change?
No, I’ve never seen this pace. I don’t see it slowing down anytime soon, either. It’s almost a call to the industry. Our industry needs help. It needs service. This is what I feel that all of us should be focused on, really engaging with these providers and helping them through the next steps. There might be 50 initiatives for even a single state, but you know what? There’s probably three that make the most sense for a practice or a cardiologist in Florida, or for an OB/GYN in Georgia.
We don’t know where the final MACRA rule will land, but I’m thinking there’s going to be some type of MIPS advancement in 2017, so we’re positioning all of our practices that way. If there is a 90-day reporting period in 2017, we want to be ready for it. I think there’s going to be. I think CMS is going to offer that option in 2017 because they don’t want to delay this until 2018.
Do you think MACRA will start on January 1 as proposed?
Here’s the way I think it’s going to play out: We get the final rule in November. I do believe that there is going to be an option that says if you want to have a 90-day reporting period, you can start July 1 and end September 30. If you want to start October 1st and end December 31st, and then report in February of 2018, you can do that. It might be voluntary in 2017, with the program really getting off the ground in 2018. It would give people time to test and to have options to see if they can perfect the process.
CMS could also say we’re going to start mandatory reporting October 1. If you want to start July 1 with the test data, that’s great, but no matter what, you have to start October 1. I wouldn’t be surprised about that, either. I think you’re going to have a 90-day reporting period in 2017, either mandatory or voluntary.
What will be key to helping physicians succeed with these new advanced payment models?
My advice is to go ahead and put a plan together for either MIPS and APM engagements or for quality reporting initiatives. Have a plan ready to go and then discuss amongst your team and board in 2016. That is the best way to position. That way, you are deliberately navigating the future of healthcare. You’re not waiting to take what balls are being thrown at you. You have proactively put a strategy in place to navigate it and see revenue increases. Again, it’s not just about surviving, it’s about thriving. I do believe that there will be more money available to you in the future than there is today if you deliberately navigate these new payment and care delivery models.
You have worked with a number of administrations over the last several years. How would you characterize each one as they related to healthcare technology? How will the next administration change the healthcare IT landscape?
Bush put the framework for strategic action into place. He’s the one who actually put this entire plan that we’re moving through in technology and innovation into place. Every single component that we are implementing today still stands on top of that framework. Then the Obama administration basically invested in that plan – institutionalizing it and making sure that we had all the necessary incentives. You have to have the infrastructure built. That’s exactly what that administration did. In 2009, it was ARRA and HITECH. Then they have layered accountable care and now MACRA on top of it. That’s the evolution of what every administration has done. Nobody has ever done it perfectly, nor will anyone ever do it perfectly because perfect is in the eye of the beholder. I’m not going to give it an A+, but they have achieved what they set out to achieve in both of those administrations.
Looking at the Trump and the Clinton campaigns, I don’t see any major changes to what has already been done. I’m not talking about a single payer healthcare system. I’m not getting into the health insurance world. In talking with staffers from both of those organizations, I’ve yet to hear anyone say, "We are going to go back to paper. We are taking IT out of healthcare. We don’t believe in shared savings. We don’t believe in risk-based contracts." There’s none of that. The fee-for-service model is no longer in healthcare’s future. I have not heard from a single person that we’re going to repeal MACRA.
This is my prediction: These programs will continue on, no matter who wins the election. I do not see a big wave of funding. I do not see anybody saying, "We need another $4 billion for this or $80 billion for that." I don’t see that at all. I do see the tying of payments to quality, value, and efficiencies in healthcare. That is what I see from both parties.
Do you have any final thoughts?
No, I think this was great. I haven’t done any real interviews since joining and being very heads down with IHealth, so I’m happy we could make this work.
Contacts
Jennifer, Mr. H, Lorre, Dr. Jayne, Dr. Gregg
More news: HIStalk, HIStalk Connect.
Get HIStalk Practice updates.
Contact us online.
Become a sponsor.














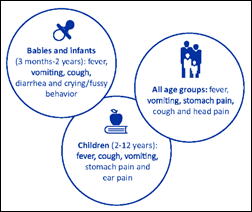

The article about Pediatric Associates in CA has a nugget with a potentially outsized impact: the implication that VFC vaccines…